Understanding Phosphorus
 AAKP wants you to learn more about “The Hidden 'P' in Kidney Disease™."
AAKP wants you to learn more about “The Hidden 'P' in Kidney Disease™."
'P' is the abbreviation for phosphorus. AAKP wants to help individuals affected by kidney disease understand the importance of knowing your phosphorus level and how high phosphorus (known as hyperphosphatemia) can cause health issues.
To learn more about National Phosphorus Awareness Day on 4.5, click here.
What is phosphorus?
Phosphorus is a naturally occurring mineral found in many foods we eat and in all living matter because it is essential for life. Although phosphorus is found in small amounts in tissues throughout the body and is involved in energy production and other body functions, next to calcium phosphorus is the second most abundant mineral in the body and is found largely in the bones and teeth. Phosphorus is an essential mineral that works with calcium to build strong bones and teeth. What else does phosphorus do?
- It is part of the body’s cell membranes, thus is important for growth, repair and maintenance of cells and tissues
- Is a component of DNA & RNA, the body’s genetic building blocks.
- Plays a role in the body’s energy storage and use: adenosine triphosphate (ATP)
- Helps maintain the pH in extracellular fluid
- Helps in the activation of enzymes
What is high phosphorus?
High phosphorus, known as hyperphosphatemia, is a condition when the phosphorus in the blood becomes elevated, or becomes higher than it should be. High phosphorus is a level above 4.5 mg/dL (milligrams per deciliter). A normal serum phosphorus level is 2.5 to 4.5 mg/dL.

How do I know if I have high phosphorus?
Your doctor can measure your phosphorus level with a simple blood test. You may not experience symptoms of high phosphorus, as high phosphorus is “silent”.

What are the symptoms of high phosphorus?
Symptoms of high phosphorus (hyperphosphatemia) are “silent” and often are undetected until abnormalities are discovered during routine blood work. Hyperphosphatemia can affect calcium levels in the bones and blood resulting in hypocalcemia, or low calcium, and the symptoms of low calcium are typically what you might feel. High phosphorus can cause serious health risks so it’s important to always check with your physician if you have any signs of hyperphosphatemia (especially if you have any of the risk factors for developing hyperphosphatemia such as CKD). Hyperphosphatemia increases risks associated with bone and mineral disease which can cause bones to become weakened or brittle, cause calcification, and damage blood vessels. To learn more about bone and mineral disease, click here.
SIGNS & SYMPTOMS OF HIGH PHOSPHORUS:
- Muscle cramps
- Brittle nails and/or dry, coarse hair
- Dry skin
- Tingling or numbness in or around the lips, tongue, fingers, or feet.
- Irritability
- Memory problems
- Abnormal heart rhythm (arrhythmia)
Hyperphosphatemia is a common condition among people on dialysis. Managing phosphorus levels can be challenging. Be your own best advocate and talk to your healthcare team about your options.

What can cause me to have high phosphorus?
There are several regulators of phosphorus, with the help of hormones such as FGF23, calcitriol, PTH, estrogen and adrenaline, and these are: the kidneys, bones, and intestines. These regulators require healthy kidneys. The most common cause of high phosphorus (hyperphosphatemia) is chronic kidney disease (CKD). Excess phosphorus is normally removed by the kidneys. If your kidneys are not working properly, phosphorus can rise to high levels.
If I develop high phosphorus, will it go away?
High phosphorus is treated depending on the underlying cause. If the high phosphorus is associated with CKD, the treatment requires continual treatment, including diet, medications, and or dialysis depending on severity of kidney damage, and monitoring by your healthcare team. Who is your healthcare team? You are the main person in your healthcare team; other members are your kidney doctor or nephrologist and your kidney dietitian. Your team might have a nurse and a social worker too!
HEALTH-RELATED CAUSES OF HIGH PHOSPHORUS
The following health conditions may increase your phosphorus level:
- Chronic Kidney Disease
- Diabetic Kidney Disease
- Hypoparathyroidism
- Low blood pH: this might be due to respiratory acidosis or metabolic acidosis
- Diabetic ketoacidosis
- Injuries: this might be associated with muscle or cell damage
MEDICATIONS THAT ARE HIDDEN SOURCES OF PHOSPHORUS
The following medications may increase your phosphorus intake and may be roughly 80 mg/day which is far lower than the phosphorus load from food additives which might be as high as 800 mg/day:1
- Calcium channel blockers
- Pain medications
- Antipsychotics
- Diabetes drugs
- Beta blockers
- Cholesterol-lowering therapy
Other medications that may increase phosphorus intake include laxatives, vitamins, and supplements. It’s vital to review over-the-counter medications and supplements with your healthcare team before use. Some medications may lead to urinary loss of phosphorus, including corticosteroids and diuretics.

What can I do to treat or manage my high phosphorus?
High phosphorus can be managed with diet changes, prescription medication, or a combination of the two. You and your healthcare team will determine the best course of treatment for you.
Nutrition Intervention
It’s important to balance good nutrition while reducing risks associated with kidney disease by slowing kidney damage. Following a low protein diet (LPD) is often low in phosphorus because phosphorus is higher and/or more “bioavailable” in high-protein foods. Phosphorus can also sneak into the diet in disguise and these hidden sources are “additives”. It’s important to know how to best reduce phosphorus in the diet by understanding that all foods are not created equal where phosphorus is concerned! We’ll review what the term bioavailable means too.
There is organic, naturally occurring phosphorus in food, and inorganic phosphorus which is not a naturally occurring phosphorus in food: this is an additive or preservative. Inorganic is a chemical that is absorbed almost 100% and causes blood phosphorus levels to increase rapidly.
Phosphorus absorption in the gut is different from different food and beverage sources:
Let’s talk about organic sources. These are food sources such as nuts, seeds, grains, vegetables, legumes, dairy foods*, fresh meat, fish, seafood, and poultry. We’ll break this group apart.
Food sources such as nuts, seeds, grains, vegetables, and legumes have the lowest phosphorus absorption, and this is due to phytate or phytic acid which is the form of phosphorus in these food products. It is very difficult for the body to digest phytate because humans do not have the enzyme (phytase) that is needed to break phytate down. This does not mean humans will not absorb the phosphorus though! As food is processed, including many cooking methods, the phosphorus becomes more “bioavailable” meaning it can be more available for absorption in the gut. The phosphorus from these food sources is absorbed ~30-50%.
Dairy products, fresh meat, fish, seafood, and poultry have organic sources of phosphorus too, but the phosphate is not bound in phytate thus can be more readily absorbable. The phosphorus in these foods is absorbed by the gut up to ~40-60% and phosphorus in milk is absorbed up to 80%.
Let’s talk a bit more about inorganic sources of phosphorus and where might you find these? Inorganic or unnatural sources or phosphorus are additives or preservatives that are found in fast foods, canned or bottled beverages, ready-to-eat or convenience foods, and enhanced meats. As mentioned, these are readily absorbable up to 100%.
Medication
Often, nutrition intervention is not enough to control serum phosphorus within the normal range. Medications might be used to help manage phosphorus levels and these are referred to as phosphate binders because the medication “binds” to the phosphorus in the gut, not allowing it to become absorbed into the bloodstream and it is then eliminated in the stool. The key to successful phosphorus lowering while using phosphate binders is the timing: it must be taken at the same time as food, or at mealtimes.
Recently a new and safe FDA-approved medication has become available which lowers phosphorus by blocking, rather than by binding, phosphorus and does not require medication to be taken at each meal, thus fewer pills are needed per day overall – which kidney patients have said helps reduce daily “pill burden.” Talk with your healthcare team to decide how best to manage your phosphorus!
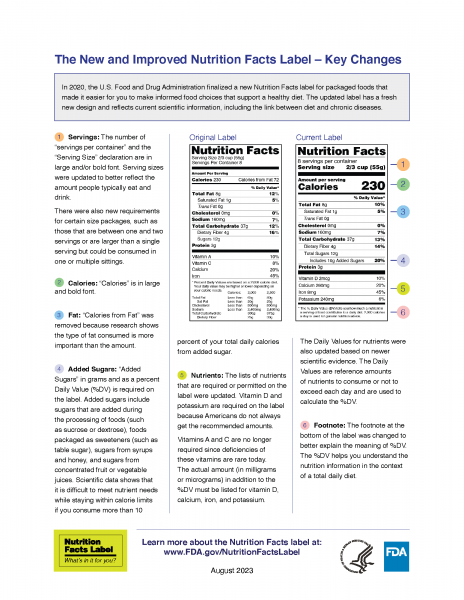
MAKING SENSE OF THE FOOD NUTRITION LABEL
The Nutrition Facts Label gives important information to all consumers. On a special diet, it can help you identify certain nutrients found in your food and how much of that nutrient it contains per serving. The following hints can help you learn how to read the read the food label.
Note that phosphorus is not listed on the food label, making it difficult for you to determine if your food or beverage choice is acceptable. One way you can find phosphorus is by looking at the ingredients for “hidden” or added sources of phosphorus. These are considered “inorganic” because they are not naturally occurring in food. Added phosphorus, or phosphate, in foods and beverages is an additive for many reasons: to extend shelf life, enhance flavors, as a stabilizer and more. Be aware of this additive because your body absorbs almost 100% of this inorganic phosphorus and can cause your serum phosphorus level to increase rapidly! You can find the hidden phosphorus by looking for words that include PHOS.
HELPFUL RESOURCES
Need help cooking low-phosphorus and kidney-friendly meals? Check out the AAKP Delicious! recipe series! All recipes are specially created for AAKP and include delicious, easy to prepare meals. Each recipe card includes a full nutrient analysis diabetic exchange and indication on what type of patient the recipe is best suited for prepared as-is. Recipe cards also feature helpful health information! Order today at the AAKP Store!
The Academy of Nutrition and Dietetics’ Find a Registered Dietitian Nutritionist online referral service allows you to search a national database of Academy members for the exclusive purpose of finding qualified registered dietitian nutritionists or food and nutrition practitioner who is right for you! Visit www.eatright.org/find-an-expert to get started!
ADDITIONAL RESOURCES:
- National Phosphorus Awareness Day (patient education resources)
- The Hidden 'P' in Kidney Disease (webinar)
- AAKP Pocket Guide to Managing Phosphorus
- AAKP Delicious! recipe series
- AAKP Pocket Guide to Understanding the Food Nutrition Facts Label
- AAKP Nutrition Counter
- AAKP Pocket Guide to Managing High Potassium (Hyperkalemia)
References
- Nelson, S. M. L., Sarabia, S. R. S., Christilaw, E., Ward, E. C., Lynch, S. K., Adams, M. A., & Holden, R. M. (2017). Phosphate-containing prescription medications contribute to the daily phosphate intake in a third of hemodialysis patients. Journal of Renal Nutrition, 27(2), 91–96. https://doi.org/10.1053/j.jrn.2016.09.007
This AAKP patient education web page is supported by an educational donation by Ardelyx. The educational content shown is unbranded and unbiased and has not been determined or influenced by any sponsor(s). It’s intended for educational purposes only.