Nearly 600,000 Americans are currently undergoing dialysis, and approximately 440,000 of them rely on phosphate-lowering therapies (PLTs) to help manage their health effectively. Because food cannot be consumed during dialysis sessions or brought into dialysis centers, patients must take these medications at home with a meal or snack — making timely, reliable access to PLTs essential.
In 2024, the leadership at the Centers for Medicare and Medicaid Services (CMS) made a significant policy decision related to PLT access that AAKP opposed. AAKP opposed their decision on the grounds that it would be detrimental to patient health and disrupt their care choice and access to PLTs. The CMS policy shift, implemented on January 1, 2025, resulted in oral-only therapies like PLTs being folded into the Part B End-Stage Renal Disease (ESRD) Medicare Prospective Payment System (PPS), commonly referred to as the "bundle payment system." This 2024 CMS policy change restricts how patients, today, access and receive these life-sustaining medications.
Recently, the full extent of the real-world consequences of this CMS policy on kidney patients became public. Kidney patients – as well as the kidney care professionals who care for them - are sharing stories of confusion, disruption, and jeopardized health. Patients are struggling to maintain consistent phosphate control since the new CMS policy rule was implemented on January 1, 2025. Read on to hear directly from those affected — and to understand what’s at stake when policy decisions limit patient choice and continuity of care.
Fighting for Health: Mihi Wickamasinghe’s Journey Managing Phosphorus on Dialysis
Mihi Wickamasinghe has been living with kidney disease since childhood. Diagnosed at just 11 years old with polycystic kidney disease (PKD), she began treatment with medication but soon went into kidney failure. For two years she managed her care through peritoneal dialysis (PD) before receiving a kidney transplant. Unfortunately, the transplant never fully succeeded. Frequent hospital stays, physical setbacks, and eventually full rejection of the transplanted kidney forced her back onto dialysis.
She stayed on PD until her body could no longer tolerate it, and today she undergoes in‑center hemodialysis (ICHD) while waiting and hoping for another transplant. Between both types of dialysis, she’s been in treatment for eight years.
“Living with kidney disease can be exhausting,” she says. “It affects every part of your life - physically, mentally, and emotionally. But I’m hopeful I’ll find a donor and get another chance at a transplant.”

Balancing Health, Work, and Education
Despite the challenges of dialysis, Mihi recently graduated from college and is now gaining work experience while planning to continue her education. “Dialysis takes a lot out of me. I’m fatigued most of the time, but I try to do my best,” she says. “Managing kidney disease while working or going to school isn’t easy.”
Learning the Importance of Phosphorus Control
Mihi first learned about the need to manage her phosphorus levels while on dialysis. Her dietitian explained the risks of uncontrolled phosphorus, including bone disease, heart complications, and even potential delays in being approved for a kidney transplant.
“She educated me on how to control my levels with diet and medication,” Mihi explains. “Both help tremendously, but it took time.”
Her treatment plan includes dietary adjustments, phosphate binders, and dialysis, all working together to keep her phosphorus within the recommended range. She checks her lab results regularly and works closely with her dietitian to make sure her level stays in the safe zone and she’s in optimal health to remain transplant ready.
CMS Imposed Barriers to Accessing Phosphate-Lowering Therapies
Since January 1, 2025, Mihi has faced frustrating delays in getting her phosphate-lowering therapies (PLTs). Because these medications are processed separately from her other prescriptions, she’s had to navigate a pharmaceutical system she wasn’t familiar with.
“My dietitian told me how to contact the pharmacy and order the medication, but it would still take longer than expected,” she says. “Sometimes I’d get less than what my doctor prescribed without any explanation, so I had to take a lower amount until the next shipment came which isn’t want my doctor or I feel is best for me or my healthcare plan.”
CMS coverage changes have also added uncertainty. Mihi was also informed that a particular PLT she was prescribed would only be available under the Medicare bundle, and policy changes could affect whether she could keep using it. She left the conversation with a sense of anxiety, uncertain whether she’d be able to continue a treatment that had been helping her and confused about how these shifting policies might impact her future care and overall health.
The Human Cost of 2024 CMS Policy Changes
For Mihi, these delays and coverage changes are more than an inconvenience - they can directly affect her ability to remain healthy and eligible for another kidney transplant. “It’s stressful not knowing if my medication will arrive on time,” she says. “But I do my part to manage my diet and take my medication as prescribed.”
She wants policymakers to understand that these therapies are not optional. “PLTs are essential for patients to live healthier lives and stay transplant-ready,” Mihi says. “We already have so much to manage. When access to medication becomes another battle, it takes a toll on our health and our peace of mind.”
For now, Mihi continues to fight, both for her health and for her future. She remains hopeful for a transplant, committed to managing her phosphorus, and determined to make sure decision-makers understand what’s at stake for kidney patients like her.
AAKP Flash Survey*: Patient, Care partner, and Healthcare Professional Insights on Access to Phosphate Lowering Therapies
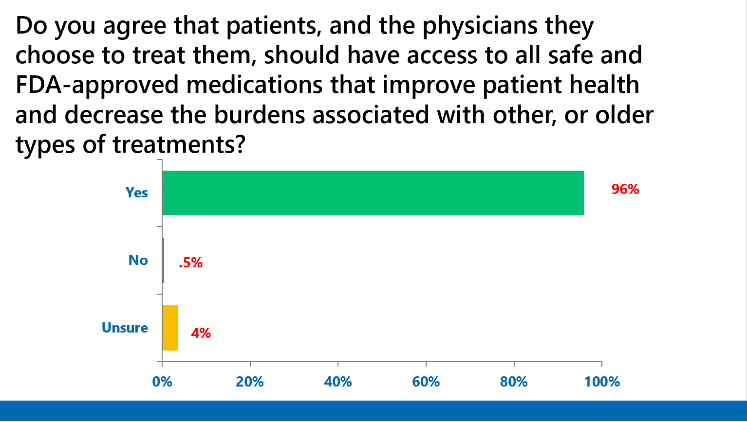
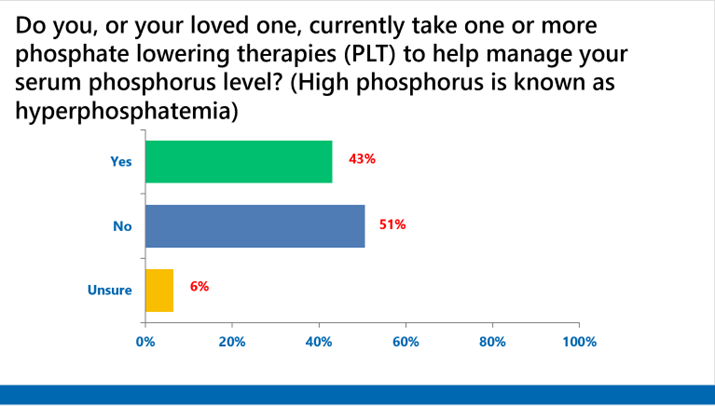
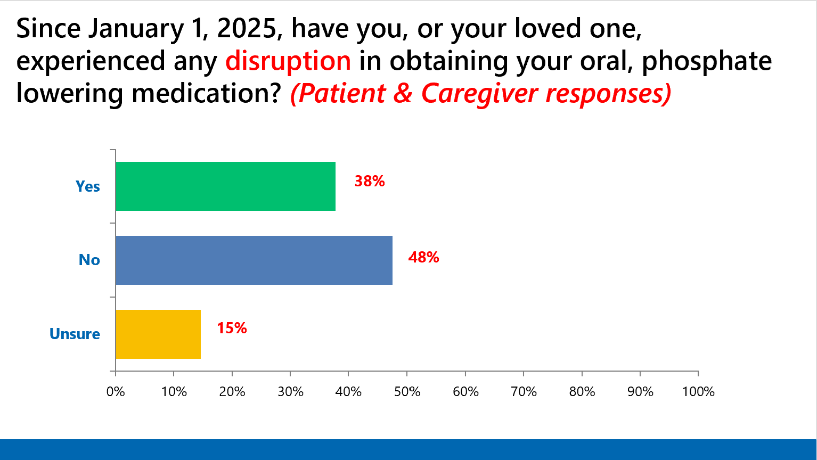
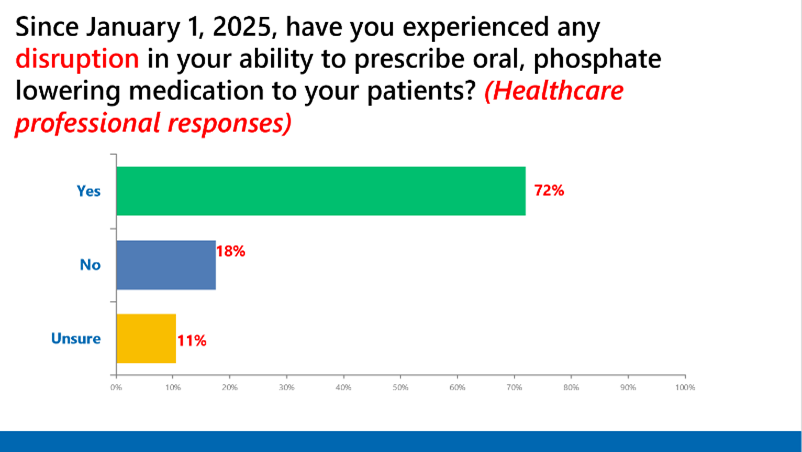
*This independent survey was conducted by the AAKP Center for Patient Research and Education. Partial survey responses are shown.
About the AAKP Center for Patient Research and Education
As part of AAKP’s National Strategy, within the AAKP Center for Patient Research and Education, we continue to expand our capacities to involve a far larger and more representative number of patients in both research and clinical trial opportunities. The results of these opportunities will help create a clearer understanding of the patient experience and can help shape the future of kidney disease treatment, care, and policies.


















