RE: FDA Proposal to Permit Salt Substitutes to Reduce Sodium in Standardized Foods
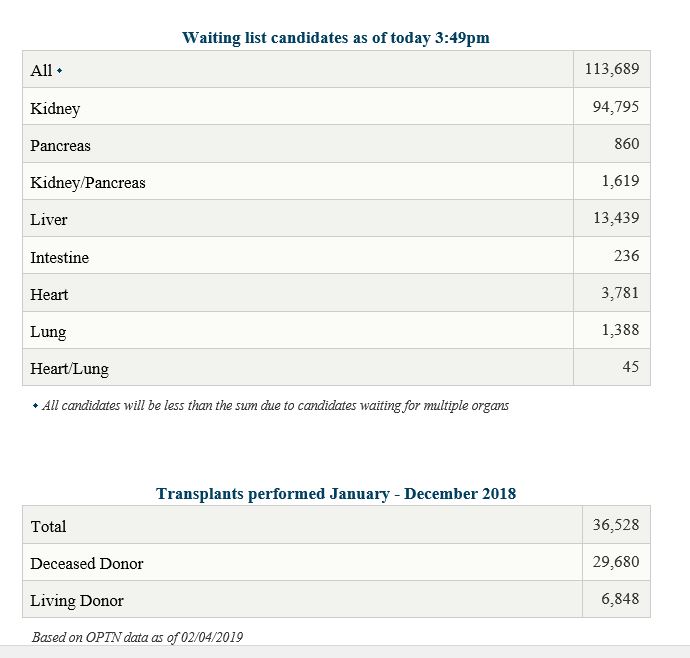
It is very important to get on the transplant list through a transplant center. In some cases, a potential recipient had a willing donor, but the center turned the recipient down because they had not gone through the testing to remain listed. Be aware of what’s required of you to also remain on that transplant wait list.
This is another great children’s book about our friend Howl the Owl (Help Others With Love) and this time he’s helping out a true Kidney Hero, Edward “YNOTT” Drake, of The YNOTT? FOUNDATION.
AAKP Ambassador, Chardae “Prima” Sanders knows the devastating effects of having high potassium. While on dialysis, Prima says that she did not watch her diet. She admits, “I was a chip eater! I would over-eat on chips. I also ate bananas as a comfort food. I never thought about the impact.”

Every morning when we awaken, our first thoughts are about how the Coronavirus is ravaging across America and the world. Each hour, more and more innocent people and their families are impacted. We also learn of the heroism of our brave first responders and selfless medical personnel. To gain strength, I think of my family and the lessons they learned from American history.

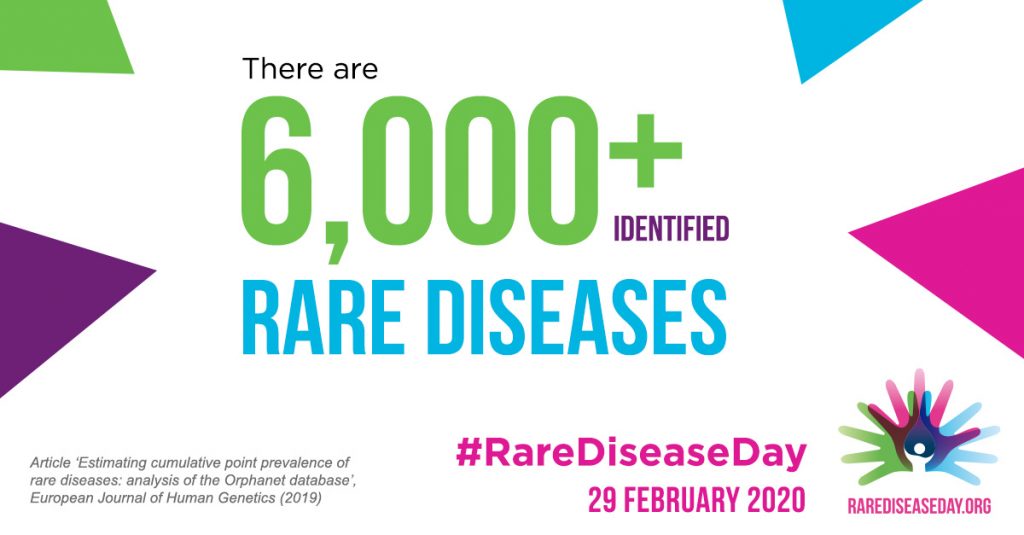
As per the NORD (National Organization of Rare Disease) website: The main objective of Rare Disease Day is to raise awareness among the general public and decision-makers about rare diseases and their impact on patients’ lives.