Nearly 600,000 Americans are currently undergoing dialysis, and approximately 440,000 of them rely on phosphate-lowering therapies (PLTs) to help manage their health effectively. Because food cannot be consumed during dialysis sessions or brought into dialysis centers, patients must take these medications at home with a meal or snack — making timely, reliable access to PLTs essential.
In 2024, the leadership at the Centers for Medicare and Medicaid Services (CMS) made a significant policy decision related to PLT access that AAKP opposed. AAKP opposed their decision on the grounds that it would be detrimental to patient health and disrupt their care choice and access to PLTs. The CMS policy shift, implemented on January 1, 2025, resulted in oral-only therapies like PLTs being folded into the Part B End-Stage Renal Disease (ESRD) Medicare Prospective Payment System (PPS), commonly referred to as the "bundle payment system." This 2024 CMS policy change restricts how patients, today, access and receive these life-sustaining medications.
Recently, the full extent of the real-world consequences of this CMS policy on kidney patients became public. Kidney patients – as well as the kidney care professionals who care for them - are sharing stories of confusion, disruption, and jeopardized health. Patients are struggling to maintain consistent phosphate control since the new CMS policy rule was implemented on January 1, 2025. Read on to hear directly from those affected — and to understand what’s at stake when policy decisions limit patient choice and continuity of care.
Fighting for His Health: A Care Partner’s View on Phosphate Management and Kidney Disease
By Susie Dantzig
When I met my fiancé 17 years ago, I didn’t know much about kidney disease. He was on peritoneal dialysis (PD), and I quickly learned that kidney failure isn’t just about the kidneys, it’s about every part of life.
Over the years, I’ve stood by him through dialysis, a living donor kidney from his sister, that transplant’s eventual failure, two more years of dialysis, and now, thankfully, a deceased donor transplant in 2023. We’ve had moments of relief, but also long stretches of exhaustion, fear, and relentless medical challenges.

Understanding Phosphorus — and Its Impact on Transplant Readiness
Phosphorus was always part of his lab reviews before the transplant. I knew it mattered, but I didn’t realize how much it could affect his ability to remain transplant-ready. High phosphorus levels can weaken bones, damage the heart, and keep a patient from being approved for a kidney transplant.
That’s where phosphate-lowering therapies (PLTs) come in, coupled with dietary changes, phosphate binders, and other medications designed to keep phosphorus in check. For patients on dialysis, PLTs aren’t “nice to have” - they are a lifeline. Without them, phosphorus levels can quickly spiral out of control, putting both health and transplant eligibility at risk.
After the Transplant — A Different Phosphorus Battle
Post-transplant, the phosphorus challenge flipped. Instead of lowering high levels, his care team now works to prevent them from dropping too low. He takes prescription medication to keep his phosphorus stable, and it’s tracked closely in his labs.
Even though his needs changed after transplant, I’ve learned just how critical PLTs are to the kidney disease journey. If access to them were ever disrupted, whether because of cost, coverage decisions, or pharmacy delays, the impact can be devastating.
Why Care Choice and Patient Access Matters
I’ve seen firsthand how hard dialysis can be on a person, physically, mentally, and emotionally. For too many people, it’s a daily struggle. If a patient loses access to PLTs and their phosphorus levels go uncontrolled, they could lose their shot at a transplant and be forced to stay on dialysis indefinitely.
As a care partner, that’s my worst nightmare. I would go to the ends of the earth to make sure my fiancé got the medications he needs. But it shouldn’t have to be that way. Patients shouldn’t have to fight through red tape, delayed shipments, or restrictive coverage policies just to get essential medications.
A Simple Message to Policymakers
For CMS leaders and Members of Congress, here’s the reality: phosphate-lowering therapies are essential to patient survival and transplant readiness. Policy changes that disrupt access don’t just affect numbers on a spreadsheet, they put real lives in jeopardy.
If the goal is to help people with kidney disease get transplanted and live longer, healthier lives, then decisions should protect and expand access to PLTs, not create more barriers.
I stand beside my fiancé every day in this fight. I only wish policymakers could stand beside us for just one of those days – they would see just how high the stakes really are.
AAKP Flash Survey*: Patient, Care partner, and Healthcare Professional Insights on Access to Phosphate Lowering Therapies
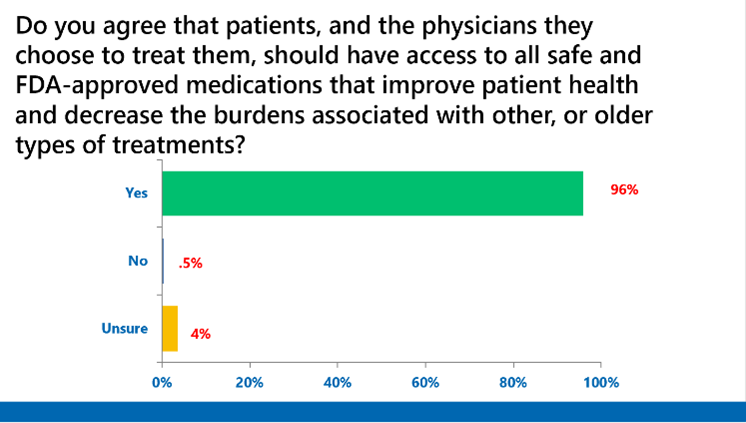
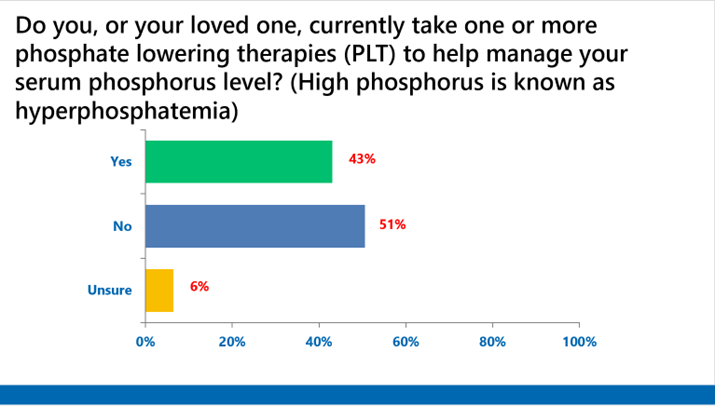
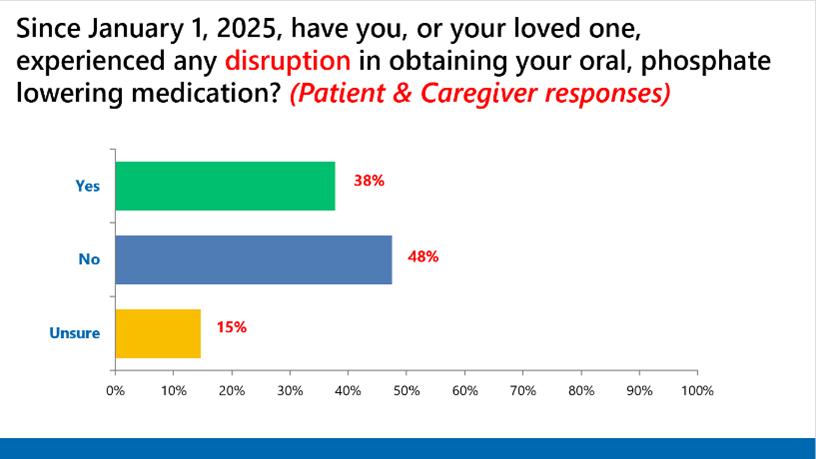
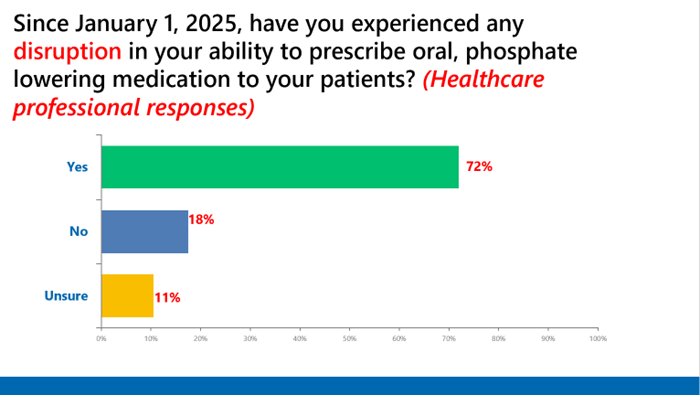
*This independent survey was conducted by the AAKP Center for Patient Research and Education. Partial survey responses are shown.
About the AAKP Center for Patient Research and Education
As part of AAKP’s National Strategy, within the AAKP Center for Patient Research and Education, we continue to expand our capacities to involve a far larger and more representative number of patients in both research and clinical trial opportunities. The results of these opportunities will help create a clearer understanding of the patient experience and can help shape the future of kidney disease treatment, care, and policies.


















