Nearly 600,000 Americans are currently undergoing dialysis, and approximately 440,000 of them rely on phosphate-lowering therapies (PLTs) to help manage their health effectively. Because food cannot be consumed during dialysis sessions or brought into dialysis centers, patients must take these medications at home with a meal or snack — making timely, reliable access to PLTs essential.
In 2024, the leadership at the Centers for Medicare and Medicaid Services (CMS) made a significant policy decision related to PLT access that AAKP opposed. AAKP opposed their decision on the grounds that it would be detrimental to patient health and disrupt their care choice and access to PLTs. The CMS policy shift, implemented on January 1, 2025, resulted in oral-only therapies like PLTs being folded into the Part B End-Stage Renal Disease (ESRD) Medicare Prospective Payment System (PPS), commonly referred to as the "bundle payment system." This 2024 CMS policy change restricts how patients, today, access and receive these life-sustaining medications.
Recently, the full extent of the real-world consequences of this CMS policy on kidney patients became public. Kidney patients – as well as the kidney care professionals who care for them - are sharing stories of confusion, disruption, and jeopardized health. Patients are struggling to maintain consistent phosphate control since the new CMS policy rule was implemented on January 1, 2025. Read on to hear directly from those affected — and to understand what’s at stake when policy decisions limit patient choice and continuity of care.
Fighting for Patient Choice: Why Access to Phosphorus Lowering Therapies Matters
When Lisa Custer, a home hemodialysis patient (HHD) from Oregon, was first diagnosed with kidney disease in her early 50s, it was during a life-threatening “crash moment” that landed her in the ER. With no known family medical history, she was adopted out of the Siletz Tribe, her diagnosis came as a shock.
That was nearly 12 years ago. Today, Lisa manages her care at home, works part-time, sings in her church praise team, and remains an active patient advocate through the AAKP Ambassador Initiative, the ESRD Networks, and the Kidney Patient Advisory Council. But her journey hasn’t been without serious challenges, especially when it comes to managing phosphorus levels.

The High Stakes of Phosphorus Management
Early on, Lisa learned the hard way what can happen when phosphorus and potassium levels spiral out of control. Both levels once climbed above 10, landing her in the ICU for three weeks. “I almost died the second time,” she recalls. Back then, she had limited dietary education and minimal training before starting home therapy.
Determined to turn things around, Lisa committed to a complete lifestyle change. She worked closely with a dietitian, eliminated unhealthy foods from her home, began exercising regularly, and meticulously tracked her meals, snacks, and blood pressure.
“Being on home therapy gives you more flexibility and frequency in treatments, which can lead to better outcomes and fewer hospitalizations,” she says. “Meal planning, timing, and portion control all matter.”
The Role of PLTs in Patient Health
For Lisa, her phosphorus medication is an essential part of her regimen. “If taken correctly, this medication can determine whether your phosphorus and potassium stay in a safe range,” she explains. “Without it, you could end up in the hospital or worse.”
Keeping her phosphorus under 5 is a constant challenge, but one that makes her feel better and healthier. Since implementation of the 2024 CMS policy change moving oral-only pills, such as phosphate lowering therapies (PLTs), into the bundle, she’s experienced delays in getting her PLTs, recently waiting over a month due to confusion and miscommunication. She’s heard from other patients who went without their medication for months, missed family trips, or were hospitalized because they couldn’t access their PLTs.
Why Patient Choice Matters
Lisa believes strongly that doctors should be free to prescribe the PLT that best fits each patient’s needs, and that patients should be able to fill their prescriptions at the pharmacy of their choice, where they can speak directly with their trusted pharmacist.
She also points out the importance of access to healthy, low-phosphorus foods, something that’s not always possible for patients facing food insecurity or living in food deserts.
The Problem with Bundling PLTs
Lisa warns that the CMS decision to move oral-only phosphate lowering therapies into the dialysis bundle beginning on January 1, 2025, has created major barriers for some kidney patients. These medications are designed to be taken with meals, not during dialysis sessions. Eating during treatment has been discouraged and even prohibited in many clinics since COVID. “To me, bundling PLTs ignores how these drugs are meant to be used and will ultimately harm patients,” she says. Her statement reflects the commonsense reaction both patients and kidney professionals are making in the aftermath of this change in policy and patient access to PLTs.
A Call to Protect Access
Lisa’s story underscores why AAKP continues to advocate for patient choice and access to PLTs. For patients like her, these therapies aren’t optional, they’re lifesaving. Ensuring timely access, respecting individual medical needs, and avoiding policy changes that restrict choice are essential to protecting better kidney health and quality of life
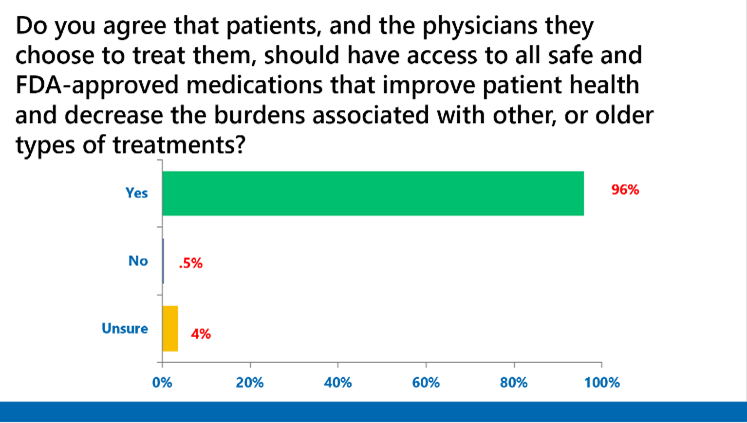
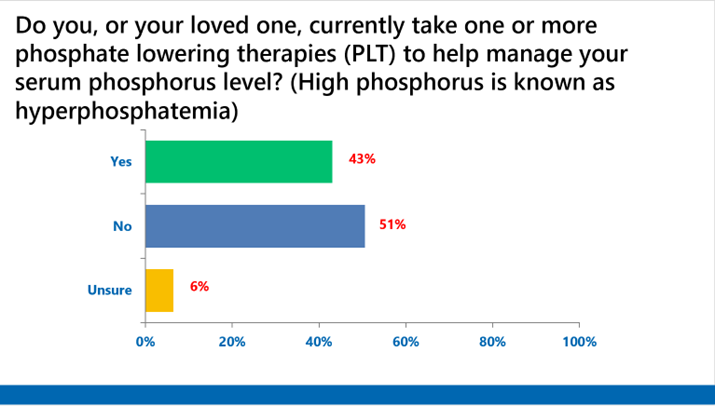
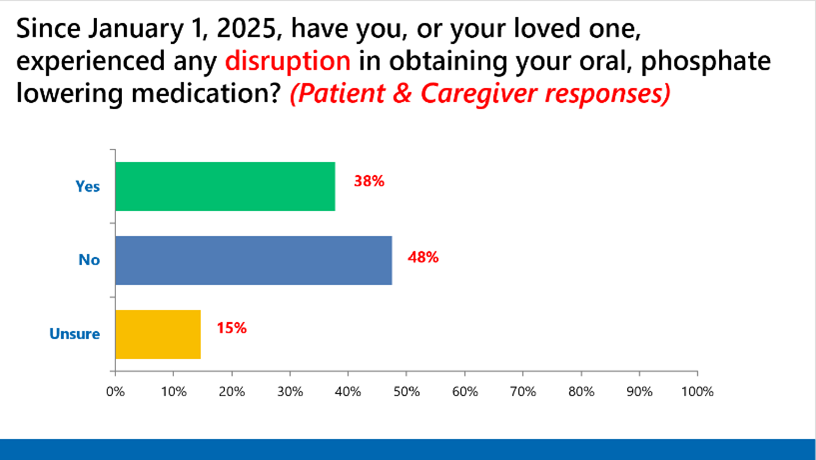
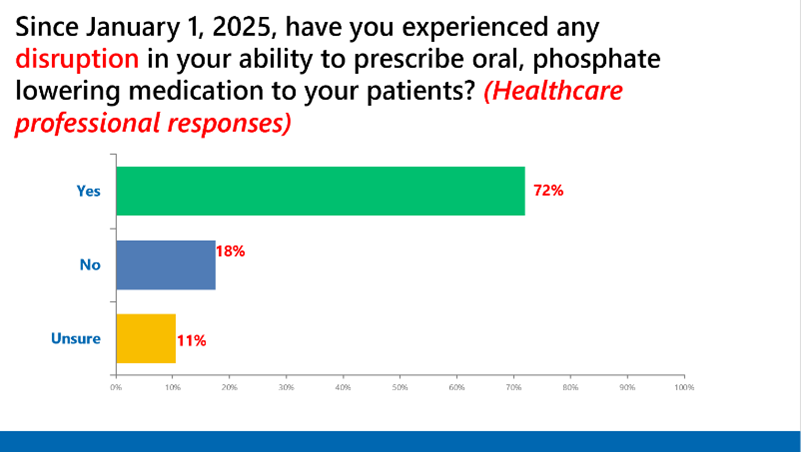
*This independent survey was conducted by the AAKP Center for Patient Research and Education. Partial survey responses are shown.
About the AAKP Center for Patient Research and Education
As part of AAKP’s National Strategy, within the AAKP Center for Patient Research and Education, we continue to expand our capacities to involve a far larger and more representative number of patients in both research and clinical trial opportunities. The results of these opportunities will help create a clearer understanding of the patient experience and can help shape the future of kidney disease treatment, care, and policies.


















