By Annamarie Rodriguez, MS, RDN, LD, DipACLM, FAND
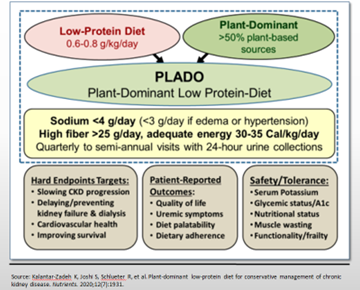
We are nearing the New Year, and many people might be thinking, “out with the old, in with the new,” and when it comes to the kidney diet this has never been truer. For the past few years, I have felt it’s celebratory when acknowledging “out” with the old, over-restrictive diet that chronically forbade persons to enjoy delicious and nutritious food and “in” with the new that is in favor of inclusiveness of grains, fruits, and vegetables! A practical approach is the use of the PLADO diet, which is a plant-dominant low-protein diet for chronic kidney disease (CKD). The PLADO diet (Figure 1) embraces plant dominance, meaning 50% or greater of the protein sources are derived from plants and the protein itself should be on the lower end to avoid hyperfiltration. The practical application of plant-based nutrition is beneficial in preventing the cause of kidney disease, reducing complications of CKD, and treating the disease itself - or at the very minimum, reducing the progression of it.
Historically, plants were thought to be avoided, but given their immense nutritional benefits, now we embrace this monumental change, and the kidney diet is moving in the direction of embracing a healthy plant-based lifestyle. Complications that occur with kidney disease include elevated phosphate levels, increased acid levels, hypertension (HTN) from the kidney disease, and elevated toxins from foods. Plant based nutrition reduces glomerular filtration rate (GFR) and reduces albuminuria(2), but can it help with those other complications?
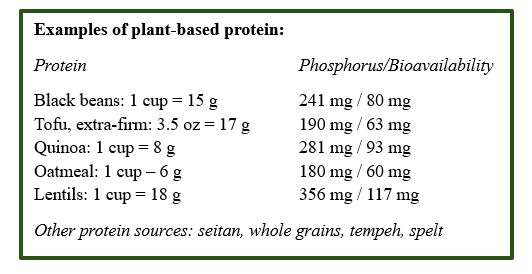
Plants, like all living matter, have phosphorus, but the bioavailability of phosphorus in plants such as grains or beans is lower than that of the phosphorus that naturally occurs in meat or milk, for example. Bioavailability refers to how much of the mineral is available for absorption in the gut. An effortless way to consider the bioavailability of phosphorus is the rule of “thirds”:
- Processed foods have a 3/3 bioavailability (100%)
- Animal-based foods generally have 2/3 bioavailability,
- Plant-foods typically have 1/3 bioavailability.(3)
It is important to know that processing and cooking methods can alter phosphorus bioavailability and that not all foods are created equally.
The American diet tends to be acidic as it is low in fruits and vegetables (F+V) which tend to be alkaline, and high in animal protein which are acidic. People with CKD struggle to excrete excess acid and maintain a normal acid-base balance. The current treatment for metabolic acidosis is sodium bicarbonate, though the same amount of alkali can be obtained by eating two to four cups of F+V and this has been shown in a number of studies in patients with CKD stages 1 – 5.(4-6) The natural alkali from F+V offers far less sodium than that of sodium bicarbonate, reducing risks of increased blood pressure and edema. Of note, in the studies, people using F+V experienced lower blood pressure, which decreased the amount of protein in the urine, and, because of the added fiber, there was a relationship with weight reduction.(7)
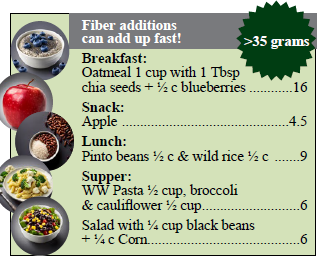
Let’s sidetrack and talk about fiber for a moment. Fiber recommendations for adults, from the Dietary Guidelines for Americans, 2020-2025, range from 22 to 34 gram (g) per day based on age and sex.(8) There are many health benefits of fiber, ranging from protective properties against cancer, heart disease, diabetes, but fiber also helps manage blood glucose for those who do have diabetes, and plays a role in gut health. Fiber types are soluble and insoluble, and both have important health benefits. Soluble fiber forms a gel-like substance and acts like a sponge to help control blood sugar and cholesterol. Soluble fiber is found in oats, apples, beans and peas, berries, kale, and more. Psyllium is a natural plant-based soluble fiber that is found in popular over the counter laxatives. Insoluble fiber does not dissolve, and it passes through the stomach keeping bowels regular and healthy. Insoluble fiber is found in whole wheat, nuts, seeds, peas and beans, and the skins of fruits and vegetables. Although fiber is known to play a vital role in overall health, just 7% of adults in the United States meet fiber recommendations, raising the risk of chronic diseases.(9)
The benefits of F+V intake correlate to an increased fiber intake which results with the reduction of uremia in the blood,(10) improved gut microbiome, reduced mortality, reduced cardiovascular disease in CKD and in one study, every extra 1 gram
of dietary fiber was associated with an 11% reduction in cardiovascular events.(11) This outcome is multifactorial as these foods have a lower acid load, promote colonic microbial activity, contain antioxidants, and are anti-inflammatory.(11,12) The PLADO diet includes a high fiber intake of >25 g/day1 making this more kidney protective. You might be wondering… “Am I getting enough fiber each day”?
Although the PLADO diet is developed for people with CKD stages 1-5, not on dialysis, this plant-dominant, high fiber approach is healthy for CKD 5D with a few adaptations. The PLADO diet is a low-protein diet providing 0.6-0.8 g/kg/day, though people on dialysis have a higher protein demand, 1.0 - 1.2 g/kg/day, and it is still easy to meet those needs using plant-proteins.(13) A worrisome concern that healthcare providers working with CKD 1-5D is potassium and, traditionally, patients have been told to avoid foods that have or are higher in potassium, which are namely plant foods. The risk may be overstated, and the reason is due to benefits associated with plants in reducing the risk of an elevated potassium, such as:(14)
Fiber ➤ associated with both bulk and frequency of bowel movements.
Colonic secretion of potassium ➤ homeostatic increase of potassium into the colon that it is excreting.
Intracellular movement of potassium ➤ associated with alkali and potential improved insulin sensitivity.
Bioavailability ➤ associated with the thickness of the plants cellular structure; the higher the fiber, the less potassium will be “available” or absorbed.
Some people, even without kidney disease, may be at higher risk of hyperkalemia and this is associated with medications (tacrolimus, ACE inhibitors, ARBs, NSAIDs, etc.), metabolic acidosis, constipation, catabolism, starvation, and wounds or tissue breakdown.(14) In a review of studies associated with CKD 1-5D and potassium, there is nearly no increase in potassium in those eating a plant-based diet.(11)
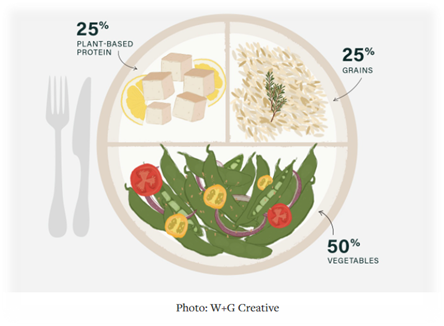
To summarize, the practical use of the PLADO diet is a useful strategy as a kidney protective nutrition intervention to minimize risks associated with CKD and slow disease progression. We might think, “OK! So how do I do it?” Figure 2 provides a guide on how many servings a day might be included and which foods to exclude, such as highly processed foods which tend to be high in sodium and minerals as preservatives, and fruit juices as these tend to be higher in potassium.(2) Use of the 50-25-25 plate rule puts the food list into perspective:
50% of the plate: nonstarchy vegetables
25% of the plate: protein foods
25% of the plate: carbohydrate foods (whole grains or starchy vegetables)
If you’re wondering how to build your plate, visit the AAKP website featuring a wealth of kidney friendly recipes: Kidney Friendly Recipes – AAKP. You’ll find a wide variety of delicious recipes for people at all stages of kidney disease and with different needs, such as diabetes or kidney transplant. There’s something for everyone whether planning your everyday meal or for special occasions!

Annamarie Rodriguez has almost 30 years of experience in a vast array of settings surrounding chronic diseases, and specifically with kidney disease. She owns Nutrition Directions, LLC providing dietitian/nutrition consulting services and is dedicated to serving the community to advocate for health equity to advance preventative measures and decrease the incidence and progression of chronic disease. She has a Master’s in Health and Wellness Management, is a Certified Lifestyle Medicine Professional, and is a Licensed Food for Life Instructor. She believes that each person is on their own personal “food journey” and the direction of nutrition care is personalized, empowering patients to sustainable life changes. She looks forward to partnering with her patients on their food journey to find the direction of nutrition that is just right for them.
References
- Kalantar-Zadeh K, Joshi S, Schlueter R, et al. Plant-dominant low-protein diet for conservative management of chronic kidney disease. Nutrients. 2020;12(7):1931.
- Joshi S, McMacken M, Kalantar-Zadeh K. Plant-based diets for kidney disease: A guide for clinicians. American Journal of Kidney Diseases. 2021;77(2):287-296.
- Kalantar-Zadeh K, Gutekunst L, Mehrotra R, et al. Understanding sources of dietary phosphorus in the treatment of patients with chronic kidney disease. Clinical Journal of the American Society of Nephrology. 2010;5(3):519-530.
- Goraya N, Simoni J, Jo C, Wesson DE. Dietary acid reduction with fruits and vegetables or bicarbonate attenuates kidney injury in patients with a moderately reduced glomerular filtration rate due to hypertensive nephropathy. Kidney International. 2012;81(1):86-93.
- Goraya N, Simoni J, Jo C-H, Wesson DE. Treatment of metabolic acidosis in patients with stage 3 chronic kidney disease with fruits and vegetables or oral bicarbonate reduces urine angiotensinogen and preserves glomerular filtration rate. Kidney International. 2014;86(5):1031-1038.
- Goraya N, Simoni J, Jo C-H, Wesson DE. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clinical Journal of the American Society of Nephrology. 2013;8(3):371-381.
- Goraya N, Munoz-Maldonado Y, Simoni J, Wesson DE. Fruit and vegetable treatment of chronic kidney disease-related metabolic acidosis reduces cardiovascular risk better than sodium bicarbonate. American Journal of Nephrology. 2019;49(6):438-448.
- Fiber: The Carb that helps you manage diabetes. Centers for Disease Control and Prevention. May 15, 2024. https://www.cdc.gov/diabetes/healthy-eating/fiber-helps-diabetes.html.
- ASN Staff. Most Americans are not getting enough fiber in our diets. American Society for Nutrition. June 9, 2021. https://nutrition.org/most-americans-are-not-getting-enough-fiber-in-our-diets/.
- Rampton DS, Cohen SL, Crammond VD, et al. Treatment of chronic renal failure with dietary fiber. Clinical Nephrology. 1984;21(3):159-163.
- Wang AY-M, Sea MM-M, Ng K, et al. Dietary fiber intake, myocardial injury, and major adverse cardiovascular events among end-stage kidney disease patients: A prospective cohort study. Kidney International Reports. 2019;4(6):814-823.
- Evenepoel P, Meijers BK. Dietary fiber and protein: Nutritional therapy in chronic kidney disease and beyond. Kidney International. 2012;81(3):227-229.
- Joshi S, Shah S, Kalantar-Zadeh K. Adequacy of plant-based proteins in chronic kidney disease. Journal of Renal Nutrition. 2019;29(2):112-117.
- Babich JS, Kalantar-Zadeh K, Joshi S. Taking the kale out of hyperkalemia: Plant Foods and serum potassium in patients with kidney disease. Journal of Renal Nutrition. 2022;32(6):641-649.


















