By Stephen Z. Fadem, MD, FACP, FASN, AAKP Medical Advisory Board Chair
When most people think about their kidneys, they imagine two quiet organs that make urine and filter waste. Important, yes—but easy to overlook. In reality, your kidneys are deeply connected to nearly every system in your body. They interact constantly with your heart and blood vessels, bones, brain, immune system, and muscles. Chronic kidney disease (CKD) is often not just a “kidney problem,” but a sign that multiple body systems are under shared stress.
Chronological Age vs. Biological Age
We usually think about age in birthdays—50, 60, 70. That is chronological age. Biological age is different: it reflects what is happening inside your cells and organs. Two people who are both 60 years old can have very different biological ages.
One way to estimate biological aging uses patterns in blood proteins. In a large study using 2,897 plasma proteins in 45,441 people, researchers identified 204 proteins that predicted age very accurately and used the “age gap” (predicted age minus actual age) to estimate faster or slower internal aging. Although this study was not designed only around kidney disease, the “age gap” tracked with kidney-function markers: a higher gap was associated with higher cystatin C and creatinine, two common blood markers tied to kidney filtration. Over 11–16 years of follow-up, people with a higher age gap had particularly high rates of osteoarthritis, followed by mortality, ischemic heart disease, type 2 diabetes, and chronic kidney disease. (1)
What Drives Biological Aging?
Several connected processes contribute to aging throughout the body—including the kidneys. (2, 3)
1) Cellular Senescence: Worn-Out Cells that Don’t Die
Some cells become damaged and stop dividing or working properly, yet they don’t die. Instead, they remain alive and release signals that can harm nearby tissue. This is called cellular senescence. These senescent cells release inflammatory chemicals known as the senescence-associated secretory phenotype (SASP), which can promote inflammation and scarring in many tissues. You can think of these as “zombie cells” because they linger and irritate neighboring cells instead of quietly disappearing. (4)
Researchers are actively exploring treatments such as senolytics that will remove senescent cells and senostatics to reduce harmful SASP signaling, though most approaches are still in development. (5)
2) Loss of Cellular Housekeeping (Autophagy) Cells normally break down and recycle worn-out parts through autophagy, a recycling process that helps prevent buildup of damaged proteins and cell components. Autophagy is influenced by nutrient-sensing pathways respond to reduced calorie intake by triggering cellular recycling.
3) Mitochondrial Dysfunction and Oxidative Stress
Mitochondria are the cell’s energy factories, producing Adenosine Triphosphate (ATP) (the body’s usable energy which you can think of as batteries). When mitochondria work less efficiently, more “leaked” reactive molecules can form, leading to oxidative stress, which can injure proteins, DNA, and membranes and can push inflammation higher. Also, the inefficient mitochondria produces less ATP and drives metabolism to produce uric acid.
4) DNA Damage and Stem Cell Exhaustion DNA is the instruction code for cells, and it faces wear and tear over a lifetime. Strong repair systems help, but if repair falls behind, cells may die or become senescent (which means to deteriorate or age). Stem cells also age, so tissues gradually lose some ability to regenerate after injury. Stem cells help repair damage, but they also age. DNA repair is essential because with all its activity, there is wear and tear that damages the fragile long chains. If the repair mechanisms fail, the cell either dies or becomes suspended and senescent, releasing Senescene-Associated Secretory Phenotype (SASP). Evidently the naked mole rat is able to extend its life to ten times other rats. One of the mechanisms is a simple mutation in a repair enzyme. In humans that enzyme, cyclic guanosine monophosphate-adenosine monophosphate synthase – luckily abbreviated cGAS, sends damaged DNA through a recycling mechanism rather than repairing it.(6) Experiences in other mammals may lead to a breakthrough in both aging, and cancer prevention.
5) Chronic Low-Grade Inflammation (“Inflammaging”)
Aging is often accompanied by persistent, low-level inflammation—even when there is no infection. This pattern is sometimes called “inflammaging.” This “background fire” may be fueled by mitochondrial stress, immune aging, senescent cells, or long-term chronic conditions. Over time it can damage blood vessels and organs throughout the body. (7)
CKD as a Reflection of Systemic Aging
Within the past two decades, the field of science that specifically focuses on aging has evolved and is known as geroscience. From a geroscience point of view, CKD isn’t just an isolated organ failure. It’s often one way the broader aging process shows itself.
Long before kidney function tests become abnormal, subtle changes can already be underway: kidney filters (glomeruli) and kidney tubules (the “processing tubes”) may lose repair capacity and gradually scar as the result of inflammation brought on by inherited genetic disorders or external factors such as high blood sugar. By the time tests like eGFR (an estimate of kidney filtering) start to fall—or albumin begins leaking into urine (albuminuria) kidney damage may already have happened “behind the scenes.” Newer biomarkers will allow us an earlier look at what is happening in the kidney with disease or aging. CKD273 is a urine-based test that looks at a pattern of 273 small protein fragments linked to kidney structure and scarring, rather than measuring kidney function at a single moment in time. Studies show that CKD273 can identify people at higher risk for developing or progressing CKD earlier than standard tests like eGFR or urine albumin alone. Because it reflects underlying biological changes in the kidney, CKD273 fits well with the idea that CKD is part of a broader biological aging process rather than just a late-stage organ failure.(8, 9)
Genetics, Epigenetics, and the Exposome
Some kidney diseases arise from single-gene conditions (for example, inherited kidney cyst disorders like polycystic kidney disease (PKD) or collagen disorders affecting the kidney filter like Alport Syndrome), but more commonly people inherit combinations of genes that increase risk for diabetes, high blood pressure, or vascular disease.
Gene activity can also be turned up or down over time through epigenetics, influenced by health conditions and environmental exposures.
What is the “Exposome”?
The exposome is the idea that your health is shaped by the total set of exposures you experience across life—diet, stress, infections, pollutants, medications, and more—interacting with your biology.
Highly processed foods, excess sodium, and certain additives can contribute to long-term metabolic stress, and some environmental or workplace toxins (such as solvents, pesticides, and heavy metals) can accumulate and disrupt normal biology over time. (10)
Common medications can matter too: frequent or high-dose use of NSAIDs (like ibuprofen or naproxen) can injure kidneys in susceptible people, especially those with existing CKD, dehydration, or multiple medications.
One Network, Many Organs
Because aging biology is shared across organs, CKD often travels with:
- Heart disease and stroke (shared vessel and pressure stress)
- Frailty and muscle loss (inflammation, toxin buildup, hormonal shifts)
- Bone disease and fractures (kidneys regulate vitamin D, calcium, phosphate, and bone-related hormones)
- Cognitive problems (vascular disease plus retained toxins and inflammation)
- Immune changes (higher infection risk and weaker vaccine responses in some settings)
CKD progression isn’t just about losing filtering units—it can reflect a body running under chronic stress, inflammation, and reduced repair capacity.
The Message: Prevention Starts Early—and Continues for Life
You don’t have to wait for an abnormal lab result to care about your kidneys. The same habits that protect your heart and brain often protect your kidneys too. Always discuss major medication, supplement, or diet changes with your clinician—especially if you already have CKD or take multiple medications. (11)
Helpful priorities:
• Keep blood pressure in a healthy range.
• Minimize added sugars and sugary drinks.
• Maintain a healthy weight and waist size.
• Limit salt and ultra-processed foods.
• Avoid smoking and get support to quit if needed.
• Stay hydrated (especially when sick, exercising hard, or in heat).
• Use NSAIDs carefully and avoid overuse.
• Exercise regularly (supports vessel health, mitochondria, and muscle).
• Eat a plant-based diet rich in fruits/vegetables and fiber (supports metabolic and gut health).

Evidence-Based and Emerging Therapies These are clinician-directed therapies showing great promise in delaying kidney disease progression:
- SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin) slow CKD progression and reduce kidney failure and heart risks in many people, including some without diabetes. (12, 13)
- RAAS blockers (ACE inhibitors or ARBs) are foundational for CKD with albuminuria/proteinuria, helping lower pressure inside the kidney filters and reduce long-term damage. (14)
- Non-steroidal mineralocorticoid receptor antagonists (finerenone) reduce kidney and cardiovascular risk in people with CKD and type 2 diabetes, beyond standard therapy in selected patients. (15, 16) The FINE One trial was just completed and the data presented at the American Society of Nephrology’s (ASN) Annual Kidney Week meeting in Houston, Texas showed that finerenone reduced microalbuminuria, a marker of kidney disease, by 25% when compared with placebo.
- GLP-1 receptor agonists (e.g., semaglutide) reduced clinically important kidney outcomes and cardiovascular death in the dedicated kidney outcomes FLOW trial in people with type 2 diabetes and CKD. (17)
- Cell-based regenerative approaches (such as investigational renal cell therapies) aim to preserve or restore kidney tissue but remain experimental and are not standard care. (18)
- Probiotics - Gut-related toxins are a growing area of research in CKD: some toxins (including indoxyl sulfate and p-cresyl sulfate) are produced by gut bacteria and may contribute to cardiovascular and systemic effects when kidney clearance is reduced.(19) (20) Strain-specific probiotic formulations such as Renadyl are showing promise in reducing the levels of known uremic toxins.(21) Probiotics are generally safe and do not require a physician prescription.
Conclusion
Your kidneys do not age in isolation; they reflect how well the entire body is maintaining balance, repair, and resilience over a several year time span. Measures of biological aging, along with kidney markers such as serum cystatin C, creatinine, and newer tools like CKD273, show that kidney changes are the early signals of the collective stress the body endures. The encouraging message is that many of the most powerful kidney-protective strategies - blood pressure management, good metabolic control, a healthy diet, regular physical activity, and avoiding toxic exposures also protect the heart, brain, bones, and muscles. We are starting to bear the fruits of lifestyle intervention with evidence-based therapies, but emerging aging-targeted treatments offer even greater hope for slowing both kidney disease and biological aging itself.
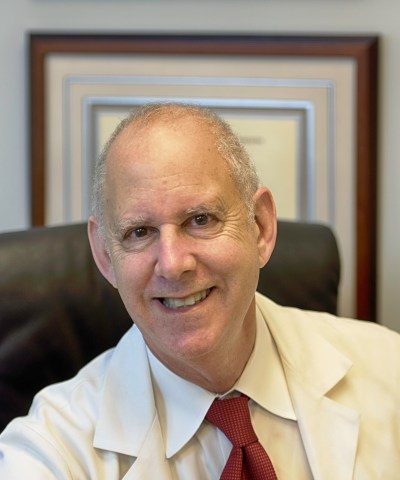
Dr. Fadem is a champion for chronic kidney disease education. He is a Clinical Professor of Medicine, Baylor College of Medicine, Section of Nephrology. Dr. Fadem attended Tulane University and graduated the University of Oklahoma College of Medicine. After he completed his internship and residency at the University of Texas Health Science Center – MD Anderson and Hermann Hospitals, he did a renal fellowship at the University of Texas Health Science Center, San Antonio. Dr. Fadem was one of the first doctors to discover the value of the Internet for patient education, and founded several websites dedicated to public service and the dissemination of clinical information including The Nephron Information Center, Wikikidney, Touchcalc and dialysisunits.com. He has participated heavily in the development and revisions of numerous AAKP patient education materials including the AAKP Patient Plan series and the AAKP Kidney Beginnings: A Patient’s Guide to Living with Reduced Kidney Function.
Dr. Fadem is the recipient of the National Kidney Foundation’s Distinguished Service Award, the AAKP Visionary Award, the AAKP Peter Lundin, MD Award, the AAKP Medal of Excellence and the President’s Volunteer Service Award. Dr Fadem is listed in America’s Top Doctors. He serves as editor of aakpRENALIFE magazine, and as historian for AAKP.
References:
1. Argentieri MA, Xiao S, Bennett D, Winchester L, Nevado-Holgado AJ, Ghose U, et al. Proteomic aging clock predicts mortality and risk of common age-related diseases in diverse populations. Nat Med. 2024;30(9):2450–60.
2. López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: An expanding universe. Cell. 2023;186(2):243–78.
3. de Cabo R, Mattson MP. Effects of Intermittent Fasting on Health, Aging, and Disease. N Engl J Med. 2019;381(26):2541–51.
4. Huang W, Hickson LJ, Eirin A, Kirkland JL, Lerman LO. Cellular senescence: the good, the bad and the unknown. Nat Rev Nephrol. 2022;18(10):611–27.
5. Afzal M, Rekha MM, Sahoo S, Pandey SN, Maji C, Goyal K, et al. Targeting the senescence-associated secretory phenotype to modify osteoarthritis in aging. Inflammopharmacology. 2025;33(11):6555–75.
6. Chen Y, Chen Z, Wang H, Cui Z, Li KL, Song Z, et al. A cGAS-mediated mechanism in naked mole-rats potentiates DNA repair and delays aging. Science. 2025;390(6769):eadp5056.
7. Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci. 2014;69 Suppl 1:S4–9.
8. Curovic VR, Eickhoff MK, Rönkkö T, Frimodt-Møller M, Hansen TW, Mischak H, et al. Dapagliflozin Improves the Urinary Proteomic Kidney-Risk Classifier CKD273 in Type 2 Diabetes with Albuminuria: A Randomized Clinical Trial. Diabetes Care. 2022;45(11):2662–8.
9. Tofte N, Lindhardt M, Adamova K, Bakker SJL, Beige J, Beulens JWJ, et al. Early detection of diabetic kidney disease by urinary proteomics and subsequent intervention with spironolactone to delay progression (PRIORITY): a prospective observational study and embedded randomised placebo-controlled trial. Lancet Diabetes Endocrinol. 2020;8(4):301–12.
10. Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement
in molecular epidemiology. Cancer Epidemiol Biomarkers Prev. 2005;14(8):1847–50.
11. Kidney Disease: Improving Global Outcomes CKDWG. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105(4S):S117–S314.
12. Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou F-F, et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2020;383(15):1436–46.
13. Empagliflozin in Patients with Chronic Kidney Disease. N Engl J Med. 2023;388(2):117–27.
14. Bhandari S, Mehta S, Khwaja A, Cleland JGF, Ives N, Brettell E, et al. Renin–Angiotensin System Inhibition in Advanced Chronic Kidney Disease. N Engl J Med. 2022;387(22):2021–32.
15. Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. N Engl J Med. 2020;383(23):2219–29.
16. Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. N Engl J Med. 2021;385(24):2252–63.
17. Perkovic V, Tuttle KR, Rossing P, Mahaffey KW, Mann JFE, Bakris G, et al. Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes. N Engl J Med. 2024;391(2):109–21.
18. Stavas J, Filler G, Jain D, Ludlow J, Basu J, Payne R, et al. Renal Autologous Cell Therapy to Stabilize Function in Diabetes-Related Chronic Kidney Disease: Corroboration of Mechanistic Action With Cell Marker Analysis. Kidney Int Rep. 2022;7(7):1619–29.
19. Falconi CA, Junho CVdC, Fogaça-Ruiz F, Vernier ICS, da Cunha RS, Stinghen AEM, et al. Uremic Toxins: An Alarming Danger Concerning the Cardiovascular System. Front Physiol. 2021;Volume 12 - 2021.
20. Sumida K, Lau WL, Kovesdy CP, Kalantar-Zadeh K, Kalantar-Zadeh K. Microbiome modulation as a novel therapeutic approach in chronic kidney disease. Curr Opin Nephrol Hypertens.
2021;30(1):75–84.
21. Natarajan R, Pechenyak B, Vyas U, Ranganathan P, Weinberg
A, Liang P, et al. Randomized controlled trial of strain-specific probiotic formulation (Renadyl) in dialysis patients. Biomed Res Int. 2014;2014:568571.


















