By Annamarie Rodriguez, RDN, LD, FAND
There is a lot of buzz around ‘plant-based’ nutrition, and the term ‘plant-based’ has evolved over the past few years; however, one thing for certain is that there is no strict definition. Plant-based nutrition can embrace the DASH (dietary approach to stop hypertension) and Mediterranean lifestyle or a Whole-Food Plant-Based lifestyle, but for now, let us focus on the PLADO approach, which is a plant-dominant, low-protein diet for persons with kidney disease.

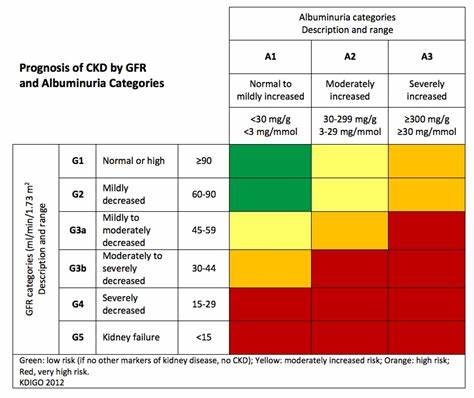
The goals of nutrition intervention and chronic kidney disease (CKD) are to decrease the risks associated with kidney disease and prevent the progression of the disease. Kidney disease continues to increase in the United States and over 35 million persons have CKD! Know your number and know your risk factors!
• 1 in 7 (or 35.5 million people) have CKD.
• 9 in 10 adults with CKD are unaware they have CKD.
• 1 in 3 adults with severe CKD are unaware they have CKD.1
There are over 800,000 persons living with end-stage kidney disease (ESKD) and compared with White people:
• Black people are nearly 4 times more likely to develop ESKD.
• Hispanic people and Native American people are more than twice as likely to develop ESKD.
• Asian people are 1.4 times more likely to develop ESKD.2
In 2018, Carolyn Crist wrote, “Diet guidance could slow kidney disease, cut costs”,3 and yet CKD continues to affect 15 percent of the US adult population.
The PLADO4 diet provides a kidney-protective approach with greater diet flexibility because although the protein intake is not truly a low protein diet (0.6 – 0.8 g/kg/day), it is a safe approach as more than 50 percent of the protein is plant-based. The plant-dominant PLADO diet is kidney protective as it is lower in sodium, higher in fiber, and it is alkaline.
We might wonder just how much protein is needed each day. The KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update reviews the following:5
• Adults with CKD on renal replacement therapy and those who have diabetes: a dietary protein of 1.0 -1.2 g/kg body weight/day.
• Adults with CKD 3-5 (non-dialyzed): a low protein diet (LPD) of 0.55-0.6 g/kg body weight/day or a very low protein diet (VLPD) providing 0.28-0.43 g/kg with additional keto acid/amino acid analogs to meet 0.55-0.6 g/kg/day is recommended.
• Adults with CKD 3-5 patients, not on dialysis who have diabetes: dietary protein of 0.6 –0.8 g/kg body weight per day.
While the jury remains out regarding what source of protein is best, plant or animal, the verdict is in regarding avoiding red meat, and processed meat and this goes for kidney disease, diabetes, cardiovascular disease, and many cancers. For those who have difficulty making changes to plant-based nutrition: consider the Mediterranean lifestyle, which is still largely plant-based. What are some examples of how much protein to include in a day? A good rule of thumb might be to consider no more than 2 ounces for each meal, and talk with your registered dietitian to find out how much is perfect for you!
For those following a very low protein diet (VLPD), the use of ketoanalogues necessary to keep the body in positive nitrogen balance; what this means is that the body will maintain an adequate amount of protein balance. Ketoanalogues have nothing to do with a keto diet or with ketosis. Ketoanalogues are an amino acid supplement that has had the nitrogen side chain removed to avoid excess nitrogenous waste build up in the blood. These are available in the United States without a prescription, and although can be costly, the cost may balance out as there is less cost burden with less protein intake.6
Protein intake and the kidneys is incredibly important in those experiencing diminished kidney function. Too much protein causes
a heavy workload on the kidneys, increases waste in the blood, and increases metabolic acidosis. This brings us to an important discussion about the kidney diet: alkalinity and acidity. Acid production in the body comes from diet, especially the Western diet, which favors animal-based foods. Plant-based foods have natural alkali that is kidney-protective. Foods that are high in dietary acid load include cheese, meat, fish, meat, and eggs.7 Fruits and vegetables are rich in alkali. It is important to balance nutritional intake with ample fruits and vegetables with minimal animal protein intake.
What makes fruits and vegetables (F+V) so exciting is they are a POWERHOUSE against inflammation because they contain antioxidants and phytochemicals. F+V has the strongest effects in the prevention of heart disease with just five servings a day! Hundreds of studies show evidence that F+V has protective effects against heart disease, and now we know that F+V decreases the risk of CKD progression. F+V promotes a healthy gut, which helps reduce inflammation, improves immunity, and reduces uremic toxins that we now know promote CKD, such as p-cresyl sulfate, indoxyl sulfate, and TMAO.8,9
Concerns surrounding F+V are often related to minerals such as phosphorus and potassium. Phosphorus occurs in the form of phytate or phytic acid in plants and is indigestible because humans truly have little phytase (an enzyme) to break this down in the gut. It must be hydrolyzed before we can absorb it and this is done through heat, processing, soaking, fermentation, and sprouting. As far as potassium is concerned, the absorption in the gut is hindered by fiber. The higher the fiber, the less potassium that will be absorbed. It is important to consider how much mineral content is in the food, but also how much may be absorbed. Another pointer to keep in mind is whether the food is natural (organic) or unnatural (inorganic). In other words, is the food processed and does it contain additives or preservatives? Preservatives that are phosphorus or potassium-based are almost 100 percent absorbed! The tried-and-true way to identify if extra phosphorus, potassium, and sodium are added to foods is to look at the ingredients on the food labels and search for “PHOS.”

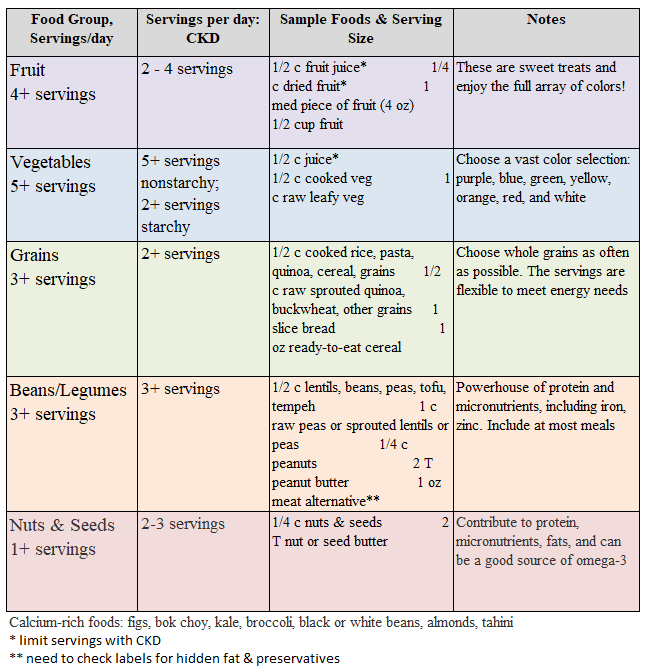
When it comes down to potassium, the fiber content is of utmost importance as fiber increases potassium excretion. Juices should be avoided, as they have no fiber. Dried fruits are very concentrated in potassium, and thus should be limited or avoided. Potassium binders can be used to help maintain potassium in normal ranges for people experiencing difficulty keeping potassium within a normal limit, thus allowing persons to enjoy these healthful, beneficial foods! There is a host of incredibly wonderful potassium education resources are available at: www.AreYouOK.org.
A transition to a LPD that is plant based and can be done easily by swaps:
• Start gradually: 1 plant-based (PB) meal per week.
• Gradually increase to 1 PB meal per day.
• Monitor bloodwork/labs and adjust.
- Review recorded intake/serving sizes with your dietitian to help make good choices and keep your labs in normal range.
• Incremental changes are easier to manage.
• Adapt familiar recipes instead of reinventing.
- Even small incremental increases in F+V are highly beneficial!
• It is all about the portion sizes = servings!
There are barriers to good nutrition, such as limited grocery choices, a tight budget, transportation, and storage. I encourage patients: do not hesitate to seek assistance. Healthcare providers must be versatile, innovative, and adapt to help suit the needs of our patients. Community partnerships must be sought in the following and we must all work together to advocate for policies to dismantle health inequities. Seek out the following to help uncover barriers and increase access to healthy food:
• Local food banks & farmers markets
• Community gardens
• Community-based centers
Healthcare providers need to make sure they assess patients for food insecurity and personalize plans that include healthy traditional foods. It’s important to brainstorm ideas with patients to promote success in meeting nutrition goals. Some things to brainstorm are:
• What are your favorite foods?
• Of the foods discussed, which ones might fit into your day?
• What types of protein do you want to eat each day?
• Which vegetables and grains do you feel you would like to try?
• Creation of cues and reminders in the daily routine to help stay on track with medication, nutrition, and activity.
Nutrition care is most successful when it is individualized and based on both personal desire and confidence!
Annamarie has worked as a nephrology dietitian for over 25 years in a variety of settings from clinical to pharmaceutical including sales, education, and renal medical affairs. She is currently an Independent Consultant, the owner of Nutrition Directions LLC, and employed by Pentec Health as a Renal Clinical Retention Specialist. She has served and chaired several boards, including the South and Central Texas National Kidney Foundation Medical Advisory Board, San Antonio Council of Renal Nutrition, the Academy of Nutrition and Dietetics’ Renal Practice Group, and several groups within the Dietetic Practice Group. Annamarie is no stranger to AAKP! She was an original reviewer of AAKP’s popular Delicious! program, which features over 100 kidney-friendly recipes.

References
1. Chronic kidney disease in the United States, 2023 -centers for disease ... Centers for Disease Control
and Prevention. May 2023. Accessed January 22, 2024. https://www.cdc.gov/kidneydisease/pdf/CKD-Factsheet-H.pdf.
2. Kidney disease statistics for the United States - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. May 2023. Accessed January 22, 2024. https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease.
3. Crist, C. (2018, August 16). Diet guidance could slow kidney disease, cut costs. Retrieved September 22, 2020, from https://mobile-reuters-com.cdn.ampproject.org/c/s/mobile.reuters.com/article/amp/idUSKBN1L12C5
4. Kalantar-Zadeh, K., Joshi, S., Schlueter, R., Cooke,
J. L., Brown-Tortorici, A., Donnelly, M., . . . Kovesdy, C. P. (2020). Plant-Dominant Low-Protein Diet for Conservative Management of Chronic Kidney Disease. doi:10.20944/preprints202005.0516.v1
5. Ikizler, T. A., Burrowes, J. D., Byham-Gray, L. D., Campbell, K. L., Carrero, J., Chan, W., . . . Cuppari, L.(2020). KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. American Journal of Kidney Diseases, 76(3). doi:10.1053/j.ajkd.2020.05.006
6. Rodriguez AM. Ketoanalogues: Not your everyday amino acids. Journal of Renal Nutrition. 2021;31(6). doi:10.1053/j.jrn.2021.08.003
7. Scialla JJ, Anderson CA. Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis. 2013;20(2):141–149. doi: 10.1053/j. ackd.2012.11.001
8. Fogelman AM. TMAO is both a biomarker and a renal toxin. Circulation Research. 2015;116(3):396-397. doi:10.1161/circresaha.114.305680
9. Mafra D, Borges N, Alvarenga L, et al. Dietary components that may influence the disturbed gut microbiota in chronic kidney disease. Nutrients. 2019;11(3):496. doi:10.3390/nu11030496
Additional Resources
Watch the 2024 Are You O-K+? The Importance of Potassium Management & Kidney Disease OnDemand at: https://bit.ly/2024AreYouOKevent


















