Good afternoon, Congressman Bilirakis. Thank you for hosting the roundtable today, and for your efforts to highlight patients’ perspectives on how to incentivize the best therapies and healthcare innovations for Floridians and for Americans. I appreciate the opportunity to join my fellow members of the roundtable discussion in sharing our stories.
My name is Janice Starling, and I am a kidney transplant recipient and former dialysis patient. My story started when I was 18 and I was diagnosed with hereditary hypertension. The older I got, the less the medication worked. During one exam, I was told I had a littler protein in my urine but it was nothing to worry about. Six months later after a family vacation I was told I had renal failure. I couldn’t believe it at first. In-fact I told the doctor he was wrong. I did not know anything about kidney disease. And then he mentioned dialysis – and that took me to another level of disbelief.
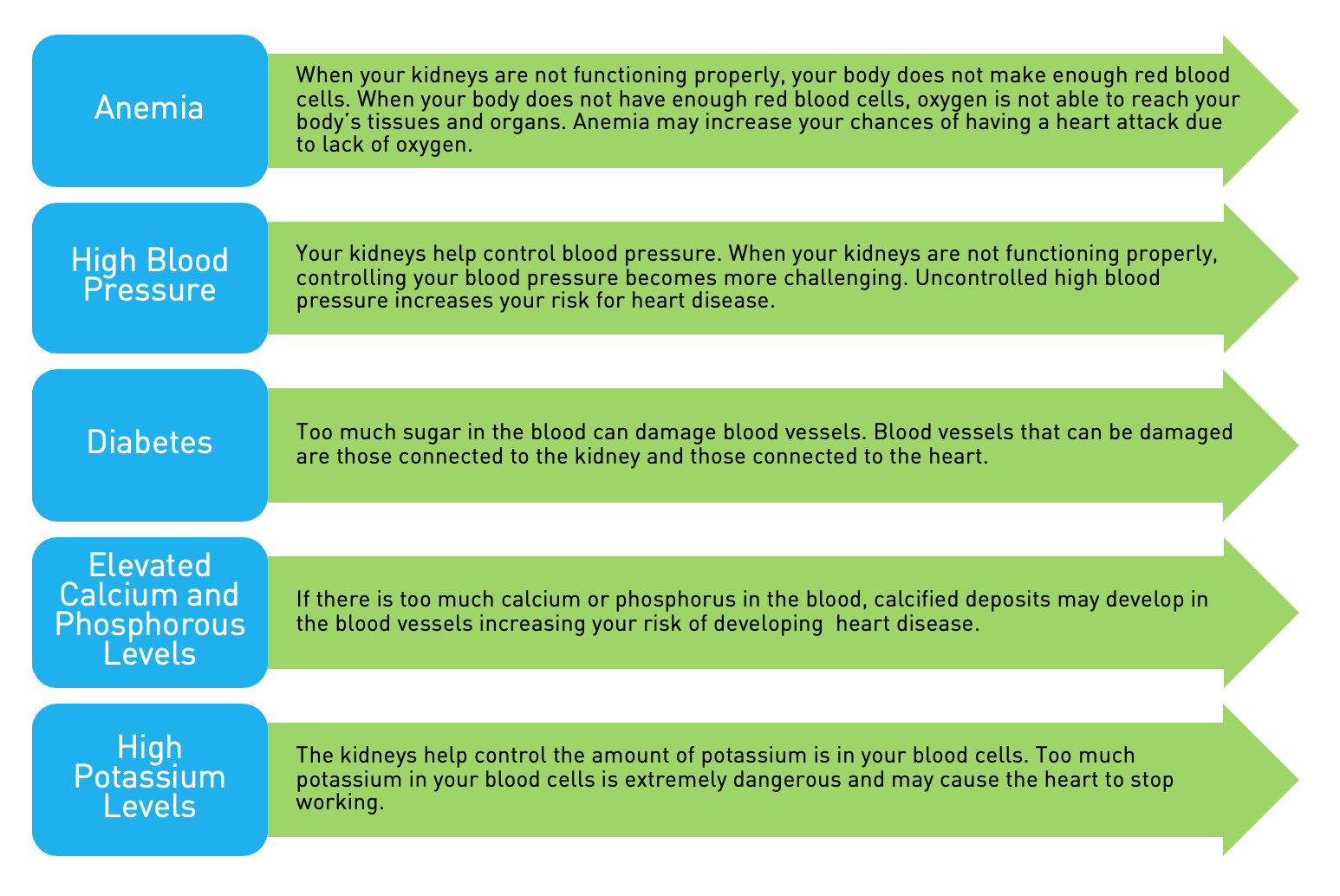
Right away I knew I had to find out more about what was going on. The hospital gave me a packet of information on kidney disease, and within that packet was information about the American Association of Kidney Patients—AAKP—which I am representing at today’s roundtable. I went on to learn that for patients with kidney failure, there are two treatments: a transplant, which I now have, is the most optimal therapy. Dialysis is the other option, and while it keeps people alive, the therapy has seen only incremental improvements since it was invented. On average, half of the people who start dialysis are not alive three years later.
Most people dialyze three days a week for about three hours, in a dialysis center. I was one of the lucky patients who were able to dialyze at home. Many US doctors don’t present home dialysis as an option at all. In contrast, many European countries present home dialysis as the first treatment of choice for kidney failure. When I found out that people could dialyze at home instead of in a center, I relentlessly asked my doctor and the staff at the dialysis center to start a home program. They were hesitant, but I kept asking and asking until they started the program.
I was a home hemodialysis patient for many years before I received my transplant. Home dialysis is so much better than in-center. It provided me freedoms that you just don’t get when you are in-center dialysis. I was able to continue to work. I served on the School Board. I was able to travel. Because I dialyzed more often at home than in-center, I was able to eat foods that I had denied myself while on in-center dialysis. My quality of life was just so much better. Unfortunately, only about 10% of patients in the US dialyze at home. AAKP is working to advocate for policies that would make it possible for more patients to have this superior option.
Recently, a coalition that AAKP is a part of asked the FDA to help allow patients to do hemodialysis at night while they sleep at home. The Alliance for Home Dialysis is asking the FDA for guidance to help the makers of nocturnal home hemodialysis machines understand the standards the FDA wants them to meet in terms of safety and efficacy, which aren’t totally clear at this time.
Nocturnal home hemodialysis uses longer and more frequent dialysis sessions than conventional dialysis. Because this more closely approximates healthy kidney—which works 24/7—it is associated with improved blood pressure, increased survival, and a better quality of life. Additionally, because patients can undergo dialysis while sleeping, nighttime dialysis provides patients with more time for daily life activities, potentially leading to societal and employment benefits. As a patient, I am disappointed that the FDA has not yet cleared any device that would facilitate nocturnal home hemodialysis.
Home dialysis is of the best improvements in kidney care—but unfortunately it is one of the only significant improvements that occurred since the invention of modern dialysis in the 1970s. In fact, there have been fewer clinical trials in kidney disease than in any other field of internal medicine. As a result, there are very few new breakthrough drugs and devices that treat kidney disease. My hope is that this roundtable, and your efforts to help improve the discovery-development-delivery process, leads to more research and new lifesaving or life-improving treatments that kidney patients need.
In lieu of a cure for kidney disease, one clear opportunity to promote better care is to help more people get a kidney transplant. More than 100,000 people are currently on the wait list for a kidney. Making it possible for more people to provide a living donation to family members, friends, and loved ones would help more people live a full life off of dialysis. Living kidney donation is safe, and people actually only need one kidney for full kidney function – it’s like everyone comes with an extra.
That is why AAKP is supporting a new bill that would allow people to take time off of work to donate a kidney. The Living Donor Act proposes to allow living donors to count under the Family and Medical Leave Act, the same law that lets new moms take unpaid time off work to give birth. Allowing people to take unpaid leave to recover and still be sure their job will be waiting for them is common-sense change that could help more people consider being a living donor.
Another bill that I hope Congress will pass will also help transplant recipients. In order to keep a kidney transplant healthy, it is imperative to take immunosuppressive drugs every day. For many patients considering a transplant, however, the cost of these drugs is a major barrier. Medicare pays for dialysis for every person regardless of age or income (approximately $90,000 per year), and then also pays for a kidney transplant (approximately $100,000). But Medicare only pays for the drugs needed to keep three years after the transplant (which cost approximately $4,000). For some patients, a $4,000 per year cost is prohibitive, so they have to stay on dialysis. AAKP is advocating for a bill in Congress—the Lifetime Immunosuppressive Drug Coverage Bill—that would provide lifetime coverage for these drugs and keep transplant recipients healthy for life.
AAKP is part of a public-private partnership with the FDA called the Kidney Health Initiative (KHI). KHI brings together patient groups like AAKP, health professional groups, scientists, industry and the FDA in order to foster the development of new kidney therapies. KHI works to eliminate some of the barriers that currently prevent the development of new kidney therapies. For instance, KHI is developing new metrics of success for clinical trials in kidney disease.
Another KHI effort currently underway is a public workshop where the FDA, the device industry, and patient advocacy groups can come together to discuss incorporating patient preferences and patient risk-benefit perspectives into product development and regulatory decisions for kidney therapies. What excites me about this initiative—and KHI in general—is that patients are involved and have been involved since the beginning. KHI is a successful model for fostering the development of new therapies, and for enabling the kidney community to interact more with the FDA.
Again, thank you for the opportunity to participate in today’s roundtable discussion. I appreciate your leadership on these important healthcare treatment and delivery issues here in Florida and in Washington, DC, and AAKP and I look forward to contributing to your efforts in any way possible. Again, thanks.