May 28, 2023
Ms. Anamika Gavhane
Senior Director
Discipline-Specific Governance
American Board of Internal Medicine
510 Walnut Street, Suite 1700
Philadelphia, PA 19106
Delivered via Electronic Mail
Dear Ms. Gavhane:
On behalf of the Board of Directors, Medical Advisory Board, and the patient and family members of the American Association of Kidney Patients (AAKP), we are honored to provide our perspective once again to the American Board of Internal Medicine (ABIM) regarding the Nephrology Specialty Board’s proposed changes to the procedural requirements for initial certification in nephrology. AAKP has consistently advocated for the principle of greater patient care choice and access to medical treatments and innovations throughout our fifty-three-year history. We are steadfast believers that patients, working closely with fully trained and ABIM-credentialed medical professionals, are intelligent consumers of healthcare who are fully capable of determining the treatments their lives – and livelihoods – depend upon.
AAKP respects the extent to which ABIM has leaned forward into the wider kidney community to gather perspectives throughout your process from other kidney stakeholders including ABIM-certified nephrologists and nephrology program directors, dialysis providers, and medical societies. As the nation’s largest and oldest independent kidney patient organization, we are extremely grateful for ABIM’s commitment to, and consistent substantive action toward, the inclusion of patient consumer perspectives in the development of certification policy and requirements. We are also very proud of our association with ABIM and the solid and unapologetic efforts Dr. Richard Baron and the ABIM team have taken over the past several years to fight for science-based medicine and to shine a very bright light on the documented disparities in care and health outcomes among underserved communities that lack true patient care choice and access to timely prevention and treatment services.
We are of the opinion that kidney disease, and its disproportionate impact among minority and rural communities, is a stark example of how paternalism and the lack of access to health education, timely treatment and care innovations has created tremendous harm and unnecessary suffering and financial hardships for far too many people and families. We believe the medical professions – especially nephrologists – can and must play an even greater role, alongside patient advocates, in changing the kidney care status quo. As national independent organizations, AAKP and ABIM are natural allies in the effort to reverse historic disparities through as many strategic policy and practice implementation mechanisms as possible.
We view updated procedural requirements for initial certification for kidney professionals as one such strategic implementation mechanism, much in the same manner that we view changes in public policy, law, regulations, and payment/reimbursement policies. We believe the closer these implementation mechanisms are aligned to kidney patient interests and unmet needs, the more progress we will make toward addressing historic disparities in both care access and health outcomes.
The ABIM Nephrology Specialty Board’s proposed changes to procedural requirements, especially those related to home dialysis, are timely and patient centered. We appreciated the work the Nephrology Specialty Board conducted to develop and make available a detailed impact statement to highlight all proposed changes. The proposed changes closely mirror our original recommendations provided in March of 2022 (attached) and as raised by Nephrology Board Member Paul Conway, our Chair of Policy and Global Affairs. Again, we appreciate ABIM soliciting, and being responsive to, kidney patient consumer concerns.
The proposed changes are also fully consistent with national kidney care policies we have been involved in at the national level for the past decade. These policies include our direct involvement in new payment models that support home dialysis and transplantation through the Center for Medicare and Medicaid Services (CMS); newly-approved home hemodialysis machines and dialysis devices, including fistulas, through the U.S. Food and Drug Administration (FDA); evolving research on potential linkages between post-dialysis fatigue and dialysis treatment modalities through the National Institutes of Health (NIH), the 2019 Executive Order on Advancing American Kidney Health, and multiple pieces of bipartisan legislation the kidney community is actively working on now with the Congressional Kidney Caucus and U.S. House and U.S. Senate leaders aimed at further prioritizing home dialysis and transplantation.
Of note, AAKP is also involved in several discussions that will lead to future Executive Orders and Executive Branch policy changes – those too will place an even further emphasis on the home setting and evolving home dialysis and remote monitoring technologies, necessitating a wider knowledge base and practical understanding of dialysis beyond current, status quo in-center treatments. One area AAKP is working on involves making home dialysis, particularly peritoneal dialysis, a more readily available care choice and consideration for kidney patients living in communities and regions that are at a known high-risk for natural disasters and unplanned events. This mirrors several critical medical and policy discussions held by the International Society of Nephrology (ISN) on World Kidney Day and at their World Kidney Congress this Spring. It is also a subject for a policy discussion at our upcoming Global Summit on Kidney Disease Innovations on June 28th, held in partnership with George Washington School of Medicine and Health Sciences, and past dialogues within the U.S. Departments of Homeland Security and Health and Human Services.
We would like to take this opportunity to offer a stretch recommendation to ABIM – and that is to make the new, proposed requirements for both home peritoneal and home hemodialysis equivalent and to the same, higher standard. We will voice strong public support for this recommendation if ABIM chooses to move it forward because we believe, based on formal and informal discussions with stakeholders, that there is support for equivalency and strong improvements to both peritoneal and home dialysis procedural requirements. We recognize that some academic institutions and dialysis providers may be resistant to higher requirements for both home peritoneal dialysis and home hemodialysis, but we believe ABIM action can facilitate greater collaborations among these stakeholders at the same federal policies and patient consumers aligning to measure progress in home therapy utilization and access.
We believe academic centers must partner with interested community nephrologists concerning End Stage Renal Disease (ESRD) care. This will have the advantage of exposing the nephrologist in training to the care in the community. Having young doctors with inquisitive minds working alongside experienced nephrologists in the community will reduce burnout, increase gratification, and give young doctors a chance to become highly proficient in caring for home patients. Many home dialysis clinics are extremely busy, and we believe many nephrologists would love to have a bright fellow work alongside them. AAKP has noticed a very high level of interest in home dialysis and remote medical monitoring among the younger generation of nephrologists, especially those interested in addressing care disparities among minority and rural populations.
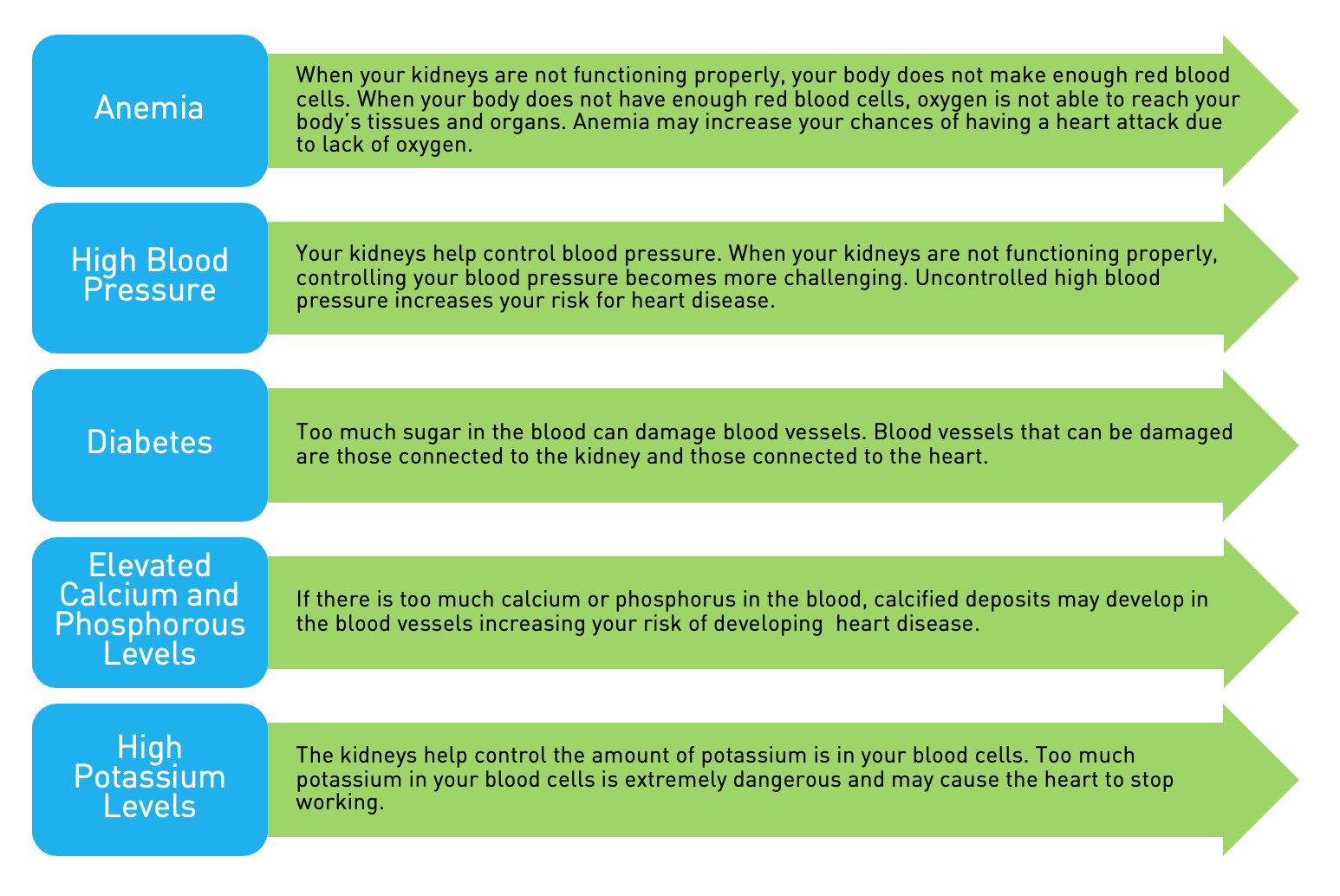
We believe that as a requirement for basic competency, nephrologists should understand all modes of renal replacement therapy, especially home peritoneal dialysis, and home hemodialysis. The AAKP has demonstrated that 31% of dialysis patients felt that the therapies were not equally and fairly represented as treatment options, and 32% were not educated regarding HHD1. This should include addressing the patient's concerns when kidney disease advances, but the patient requires therapy. It should include an understanding of the mechanics of dialysis, how to support the training program, and how to diagnose and treat complications of care.
This will have a strong and positive impact on the care kidney patients now receive. Many are not introduced to home modalities early in their care and progress to the point that they need dialysis on an emergency basis. Their first dialysis is in the hospital, and they are discharged to an outpatient hemodialysis center with a catheter. Nephrologists need to be trained to work as a team with primary care physicians to identify patients who will need further care and help prepare them for either a preemptive transplant or a home dialysis modality.
A well-trained patient who dialyzes at home retains independence. The labor costs and total care costs are substantially reduced when patients perform their own care. Patients who are dialyzing at home, (or better still, who have preemptive kidney transplants) can continue working in part-time and full-time jobs and remain productive members of their families and their community. This promotes self-esteem and reduces depression. This is a particular area of interest for AAKP and a growing area of interest and collaboration with NIH researchers, and the U.S. Department of Labor’s Office of Disability Employment and other federal and state agencies.
AAKP defines high quality healthcare as medical care and treatment that best aligns to the aspirations of patients, and we believe that kidney patients have the same aspirations and deserve the same opportunities as any other American, regardless of their socio-economic background or disease status. This means the opportunity to pursue meaningful part-time and full-time work in a trade or profession of their choosing and consistent with their training and education, the opportunity to own a home, start a family, and to retire securely. We reject the idea that chronic kidney disease, kidney failure and dialysis treatments must be accompanied by a life marked by unemployment, dependency, and disability – but as patients and patient advocates, we are also observant and wise enough to know these conditions are often directly related to a prescription for in-center dialysis care. Unfortunately, these conditions, or side effects, are not always explained to patients before they are placed on that type of dialysis therapy.
We appreciate the opportunity to offer our robust endorsement and full support of ABIM’s proposed changes to the procedural requirements for initial certification in nephrology and hope you also consider our stretch recommendation to make the new procedural requirements for peritoneal and home hemodialysis equivalent – to the highest standard.
Sincerely,

Edward V. Hickey, III
AAKP President
Chair, Veterans Health Initiative
Chronic Kidney Disease Patient
Cc:
Richard V. Knight
Immediate Past President
Former Dialysis Patient, Current Transplant Recipient
Stephen Fadem, MD, FACP, FASN
Chair, Medical Advisory Board
Diana Clynes
Executive Director
AAKP Board of Directors
Attachments:
Topline AAKP Comments re: Procedural Requirements for ABIM Certification in Nephrology (As delivered during the ABIM Board Meeting of March 25, 2022 by AAKP Chair of Policy Paul T. Conway)
- Fadem, Stephen Z.*; Walker, David R.†; Abbott, Greg†; Friedman, Amy L.‡; Goldman, Richard§; Sexton, Sue†; Buettner, Kim‖; Robinson, Kris‖,a; Peters, Thomas G.¶. Satisfaction with Renal Replacement Therapy and Education: The American Association of Kidney Patients Survey. Clinical Journal of the American Society of Nephrology 6(3):p 605-612, March 2011. | DOI: 10.2215/CJN.06970810