By John Laisure, PA-C, Pediatric Nephrology (kidney) and Hypertension Clinics, Brenner Children’s and Atrium Health Wake Forest Baptist
120/80? How does my child have high blood pressure (hypertension)? I thought that was normal. Why does my child’s doctor keep changing what normal blood pressure should be? Why am I seeing a kidney specialist (nephrologist) for blood pressure issues?
These are questions I get all the time as a Physician Assistant in the Pediatric Nephrology (kidney) and Hypertension Clinics at Brenner Children’s and Atrium Health Wake Forest Baptist. Not only do I have the privilege to help my patients and families try to navigate their high blood pressure diagnosis, but I have also experienced this personally as a patient.

I was 18 years old when I was diagnosed with Polycystic Kidney Disease (PKD). PKD is a genetic disease that causes fluid-filled cysts to form in the kidneys. Over time, these cysts grow and cause the kidneys to enlarge, ultimately leading to kidney failure requiring dialysis and/or kidney transplant. A common complication of PKD is high blood pressure. At a young age, I got used to monitoring my blood pressure regularly and taking medicine daily to help keep my blood pressure in the normal range. Was it hard? Yes! I would be annoyed having to set alarms and reminders to take the medication every day. It was frustrating having to remember to take my blood pressure regularly. Any time I left for vacation or camp, I needed to pack enough medication to last the entire trip. In 2017, I was fortunate to receive a kidney transplant from a gracious living donor. That helped solidify my passion for caring for kids with kidney disease; I love connecting with my patients and their families every day, knowing firsthand what it’s like to go through these difficult periods.
The kidneys play an important role in your body’s blood pressure control. The kidneys regulate the water and salt balance in your body by producing several hormones and enzymes which communicate with the rest of your body. When the kidneys are damaged, their ability to balance water and salt in your body is disrupted and leads to relatively too much water and salt being retained and thus raising your blood pressure. Other common factors also contribute, including obesity, congenital heart diseases, and endocrine diseases affecting the thyroid or adrenal glands that produce similar blood pressure-regulating hormones.
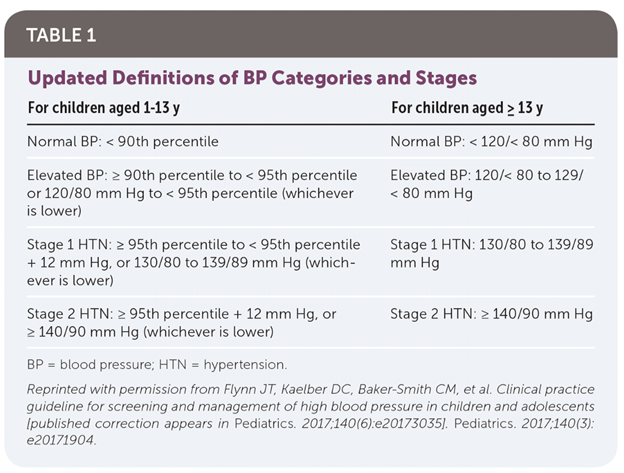
The normal range of blood pressure varies by age, gender, and height. On average, blood pressure is normally higher in older kids, boys compared to girls, and taller kids compared to shorter kids. That is why your child’s blood pressure goals often change based on how much they grow each year. For kids aged 12 years old and younger, we use normal percentiles to account for age, gender, and height that were set by the experts in the field. Your child’s nephrologist should provide you with your child’s normal blood pressure goals at each visit and support you in being able to monitor blood pressure at home. Indeed, as providers in the Hypertension Clinic, we value out-of-office blood pressure measurements, including at home and school. These measurements give us a better understanding of your child’s true blood pressure over time. In teenagers 13 years old and above, we follow the same blood pressure goals as adults.
There are three different levels of high blood pressure—elevated blood pressure (previously called prehypertension), stage 1 hypertension, and stage 2 hypertension. The following table shows how the percentiles for height, age, and gender are used to categorize normal versus high blood pressure.
It is crucially important to measure your child’s blood pressure correctly so that it is accurate. Using the wrong size cuff can falsely raise (if too small) or falsely lower (if too large) your child’s blood pressure. There are markings on each blood pressure cuff to help determine the appropriate size to use; the size often increases as your child grows. If you have any questions, ask your child’s healthcare team. It is important for your child to rest for about five minutes before taking their blood pressure and sit relatively still while taking their reading.
In a busy clinic, sometimes it is hard to get an accurate blood pressure when you are rushing from a busy parking garage or trying to make it on time to your appointment—that is okay! We all try our best to get as accurate a measurement as possible. That is why it is important to recheck a child’s blood pressure after the child has been calm and sitting in the room. When blood pressure is being measured, they should have their feet flat on the ground and legs uncrossed. The provider will often take several measurements to ensure they record the most accurate numbers.
During the initial evaluation for high blood pressure, we also assess for any other causes throughout the body that could be causing the high blood pressure. This typically involves urine tests, blood tests, and ultrasounds of the heart and kidneys. Treatment with medication depends if there are any abnormalities seen on this initial workup. If we find no specific cause of high blood pressure, we label it as primary hypertension.
Our goal in the Hypertension Clinic is to work with you and your child to help your child be as healthy as possible for as long as possible. That is why our first goal in managing all our patients with high blood pressure is lifestyle counseling—eating more nutritious foods and being more physically active. Eating too much salt can raise blood pressure significantly. When most people think of salt, they just think of the saltshaker on their kitchen table. However, there are many other sources of salt, also called sodium. Frozen, processed, and fast food often have high levels of sodium because it is a great food preservative. Condiments such as ketchup and hot sauce also are high in sodium. The recommended daily sodium intake in the United States is <2300mg/day regardless of age. The average intake is 3300mg/day in 6 to 18-year-olds. For example, a fast-food kid’s meal usually has over half (more than 1000mg+) of your child’s recommended daily sodium intake. We encourage our patients and their families to meet with our trained dieticians to go over what they eat in detail to find what I call “hidden salt” that you may not think of.
If lifestyle management does not improve blood pressure enough, our next step of action is based on what level of high blood pressure the patient is in. If the blood pressure is in the elevated range, we continue to monitor over time and continue to encourage healthy lifestyle changes. If the blood pressure remains at stage 1 or 2 despite incorporating lifestyle management, your provider will discuss with you the appropriate medication to start your child on. Common indications to initiate medication is if your child is symptomatic—headaches, chest pain, and heart palpitations. Also, any abnormalities seen on the kidney or heart imaging that would indicate it is from hypertension. Finally, if your child has co-morbidities such as obesity, diabetes, or heart disease, this can lead us to start medication. There are many different kinds of blood pressure-lowering medications that we can use to help control blood pressure, and the vast majority of them are very well tolerated by kids with minimal to no side effects. Most kids are able to still participate in their regular activities without any issues. The medications work by blocking various hormones that raise blood pressure and help correct the body’s water and salt balance.
Once a medication is started, we work with your child and you to keep the blood pressure controlled for at least a year. If the blood pressure is maintained at a normal level and there are no concerning findings in the lab work or repeat imaging, we slowly decrease the dose until they no longer need it. I always tell patients that our hope is that the blood pressure will come down on its own through lifestyle management, but that the medication is a terrific helper along the way. Even small changes in what we eat—such as cutting out fast food, increasing water intake, and increasing physical activity—can go a long way towards lowering and even normalizing blood pressure. Your child’s provider will make specific recommendations for your child and work with you to make the best decisions to manage their blood pressure.
I can still remember back to the first time I saw 130/90 on my home blood pressure machine as a teenager and the feelings and questions that came along with it. My nephrologist at the time was very understanding and answered all my questions. I now hope to bring that same comfort and understanding to my patients. We are here to help!
If you would like additional information about the Hypertension Clinic at Brenner Children’s and Atrium Health Wake Forest Baptist, please visit https://www.wakehealth.edu/condition/p/pediatric-hypertension.
John Laisure is a Physician Assistant in the Department of Pediatrics-Section of Nephrology at Brenner Children’s and Atrium Health Wake Forest Baptist. His interests include hypertension and kidney transplant, along with cystic kidney disease.