The prevalence of sleep disorders in the United States is exceedingly high. Sleep disorders cause a high number of health problems, are associated with high healthcare costs and are frequently linked with cuts in quality of life that negatively impact social and work relationships.
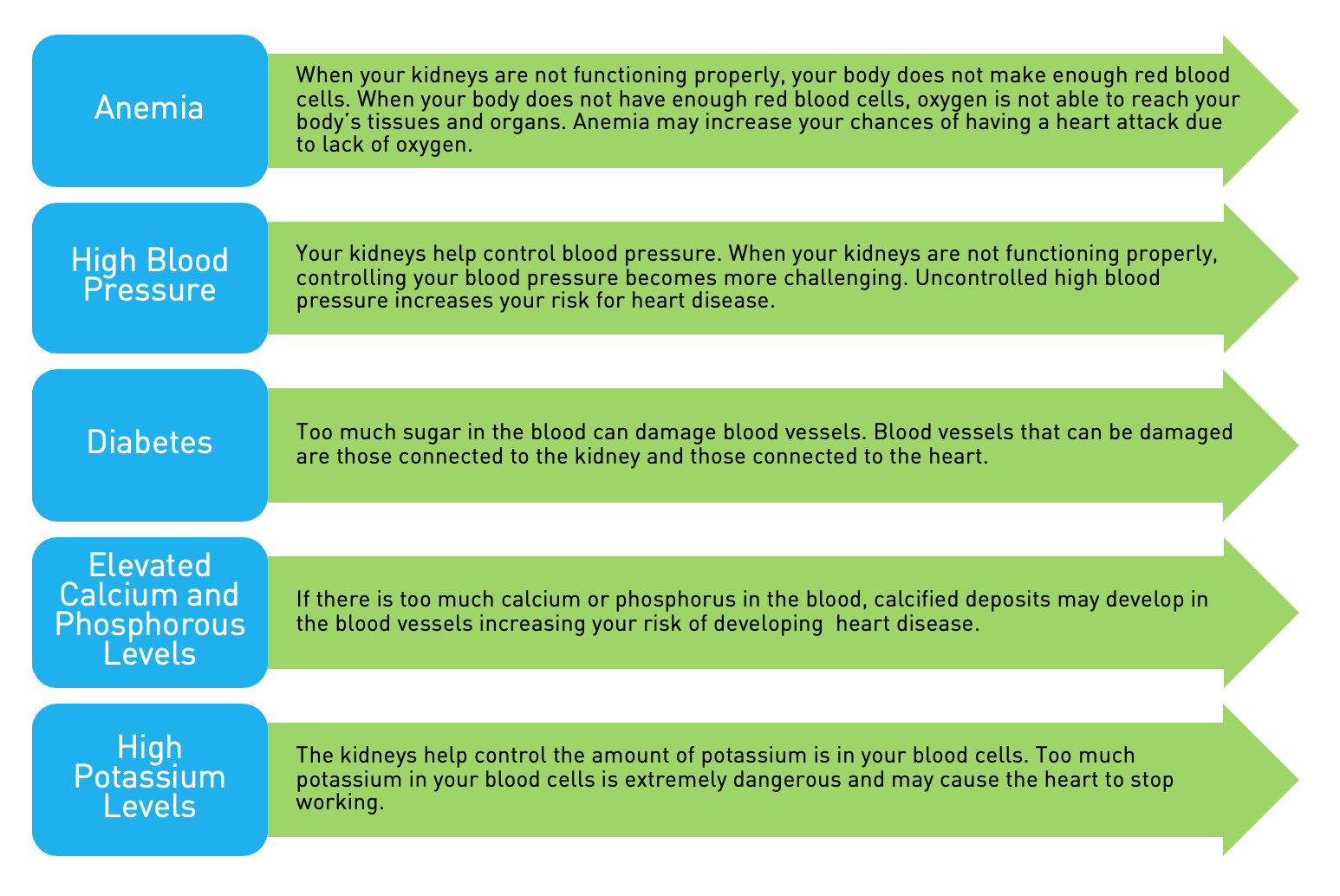
In particular, chronic kidney disease (CKD) is extremely common in older individuals affecting up to one in five Americans over 65 years of age, and we know there is also an increasing prevalence of sleep disorders, such as insomnia and sleep apnea, with increasing age. Traditional cardiovascular risk factors such as diabetes, hypertension, hyperlipidemia (elevation of fats in the bloodstream) and smoking explain part of this risk. Factors resulting in sleep disruption, such as sleep apnea, are commonly associated with CKD and may also play a role. It is reasonable to consider the treatment of sleep disorders, such as sleep apnea, in CKD may improve morbidity and mortality in this setting.
Sleep disturbances and sleep disruption are very commonly observed in patients with CKD. Most studies and investigations to date have examined patients with end-stage renal disease (ESRD) on dialysis. Sleep complaints have been noted to occur in up to 80 percent of dialysis patients, and literature supports reduced sleep, sleep fragmentation and increased wakefulness after falling asleep is common in those on dialysis. Data in one study also shows approximately 50 percent of the dialysis patients complained of problems with sleep, as opposed to only 12 percent of healthy individuals. Some of the most common sleep complaints reported include nighttime awakenings in 67 percent, early morning awakenings in 80 percent, restless legs syndrome (RLS) symptoms in 72 percent, jerking legs in 83 percent and daytime sleepiness in 28 percent of patients. Dialysis patients also experience changes in their recorded sleep architecture. Polysomnographic (record of sleep pattern) features include reduced total sleep time, reduced sleep efficiency (total sleep time/time in bed, normal >90 percent) as low as 66 percent, and increased amounts of wake time during the sleep period. In addition, specific sleep disorders such as sleep apnea, RLS and insomnia have been reported to be very common in the setting of CKD. Polysomnographic studies have also demonstrated that sleep architecture (the composition of sleep stages during sleep) is usually abnormal, with increased amounts of stage 1 (lighter stage of sleep) and 2 sleep, and decreased amounts of stage 3, 4 (deep sleep) and REM sleep (the latter thought to play a role in memory consolidation). The progression of kidney disease has also been associated with the progression and worsening of sleep difficulties and sleep quality. Interestingly, in a recent study published this year, the prevalence of sleep disorders as ascertained by a questionnaire within two months of the diagnosis of mild renal dysfunction (mean creatinine level=2) was 89 percent, suggesting even those patients with mild kidney disease not on dialysis are prone to having sleep difficulties.
CKD and Sleep Apnea
Sleep apnea is a disorder characterized by repetitive, intermittent upper airway collapse resulting in upper airway obstruction. The prevalence of sleep apnea in the United States population is estimated to range from 2-4 percent with higher prevalence in men compared to women. Typical symptoms observed in sleep apnea include snoring, witnessed apneas (episodes of breathing cessation) noted by the bed partner and excessive daytime sleepiness.
In pre-dialysis patients the prevalence of sleep apnea is very common (50 percent), and affects up to 80 percent of individuals on dialysis.
Nocturnal hemodialysis has been shown to improve sleep apnea in those with ESRD with some data supporting mechanisms of an increase in pharyngeal airway size. It is thought ESRD is associated with increased narrowing of the airway likely due to pharyngeal edema (fluid in the tissues of the airway) which may increase the likelihood of sleep apnea. Treatment with nocturnal hemodialysis may help decrease this fluid and therefore improve sleep apnea. The relationship of sleep apnea with CKD is thought to be bi-directional, meaning CKD-associated changes in fluid shift, acid-base balance and chemoreflexes may predispose someone to sleep apnea. Conversely, sleep apnea-related hypoxia, increased carbon dioxide levels and increased sympathetic nervous system activity (fight or flight response) could lead to worsening kidney disease. Sleep apnea through the mechanisms described is also a risk factor for cardiovascular disease by increasing systemic inflammation, oxidative stress and vascular (blood vessel) function. The recognition and treatment of sleep apnea in CKD must be emphasized in order to reduced cardiovascular risk and potentially minimize progression of renal disease in CKD.
CKD and Restless Legs Syndrome (RLS)
Patients who have ESRD also have a high prevalence of RLS and periodic limb movements. RLS is characterized by unpleasant, restless sensations in the legs, arms, hands or feet and an irresistible urge to move those body parts. Not all patients experience the same symptoms with some noting an itchy sensation while others note a creeping or crawling feeling. In some cases symptoms may consist of painful burning, prickling or aching. These symptoms are typically worse in the evening and with prolonged immobility (such as during dialysis), and can often be improved by movement. Up to 80 percent of patients who have ESRD experience symptoms consistent with RLS. In addition, sleep study recordings of sleep patterns have demonstrated a high prevalence of period limb movement disorder (PLMD), a condition during sleep characterized by episodic limb movements in association with disrupted sleep. PLMD affects up to 70 percent of the dialysis population. What leads to RLS and PLMD remain unknown, although it has been speculated that iron, folate and vitamin B12 deficiencies could predispose hemodialysis patients to these disorders. In addition, low plasma levels of tyrosine, which is the amino acid precursor of dopamine, have been observed in uremic patients, and it is widely believed RLS may result from dopamine deficiencies in the central nervous system. Disorders that commonly coexist with CKD such as anemia and diabetes mellitus may also represent the cause for RLS symptoms.
CKD and Insomnia
Chronic insomnia is a common sleep disorder estimated to occur in 10-15 percent of the population. In one study based upon self reported questionnaire data, close to 43 percent of individuals with mild CKD had sleep onset insomnia defined as a sleep latency of greater than 30 minutes (meaning it took 30 minutes or longer to fall asleep) and 63 percent reported sleep maintenance insomnia symptoms characterized by repetitive nocturnal awakenings disrupting sleep. Insomnia symptoms in CKD could also represent another sleep disorder such as sleep apnea presenting as sleep maintenance insomnia due to sleep disruption or RLS presenting as sleep onset insomnia.
Conclusion
Sleep disruption and sleep difficulties as well as specific sleep disorders such as sleep apnea, RLS and insomnia are common in those with CKD. It is important to note that the recognition, diagnosis and treatment of these disorders are extremely important to improve cardiovascular and overall health status as well as quality of life.
Reena Mehra, MD, MS, FCCP, DABSM, is an Assistant Professor of Medicine in the Division of Pulmonary and Critical Care Medicine and the Division of Clinical Epidemiology and the Medical Director of the Adult Sleep Laboratory of the University Hospitals of Cleveland.
This article originally appeared in the November 2008 issue of aakpRENALIFE.