By Melissa Bensouda, AAKP Ambassador

Photo: Representing Missouri at RPA Advocacy Day on Capitol Hill –
Dr. Gary Singer, MD; Melissa Bensouda, AAKP Ambassador MO; Kinza Bensouda (daughter)
At one point in my childhood I had dreamed of becoming a nurse. That dream quickly changed when I learned about the “behind the scenes” things nurses did to care for sick patients – my stomach wasn’t cut out for it. I would have never imagined that my desire to help sick patients would now be best used to save my own life with home dialysis.
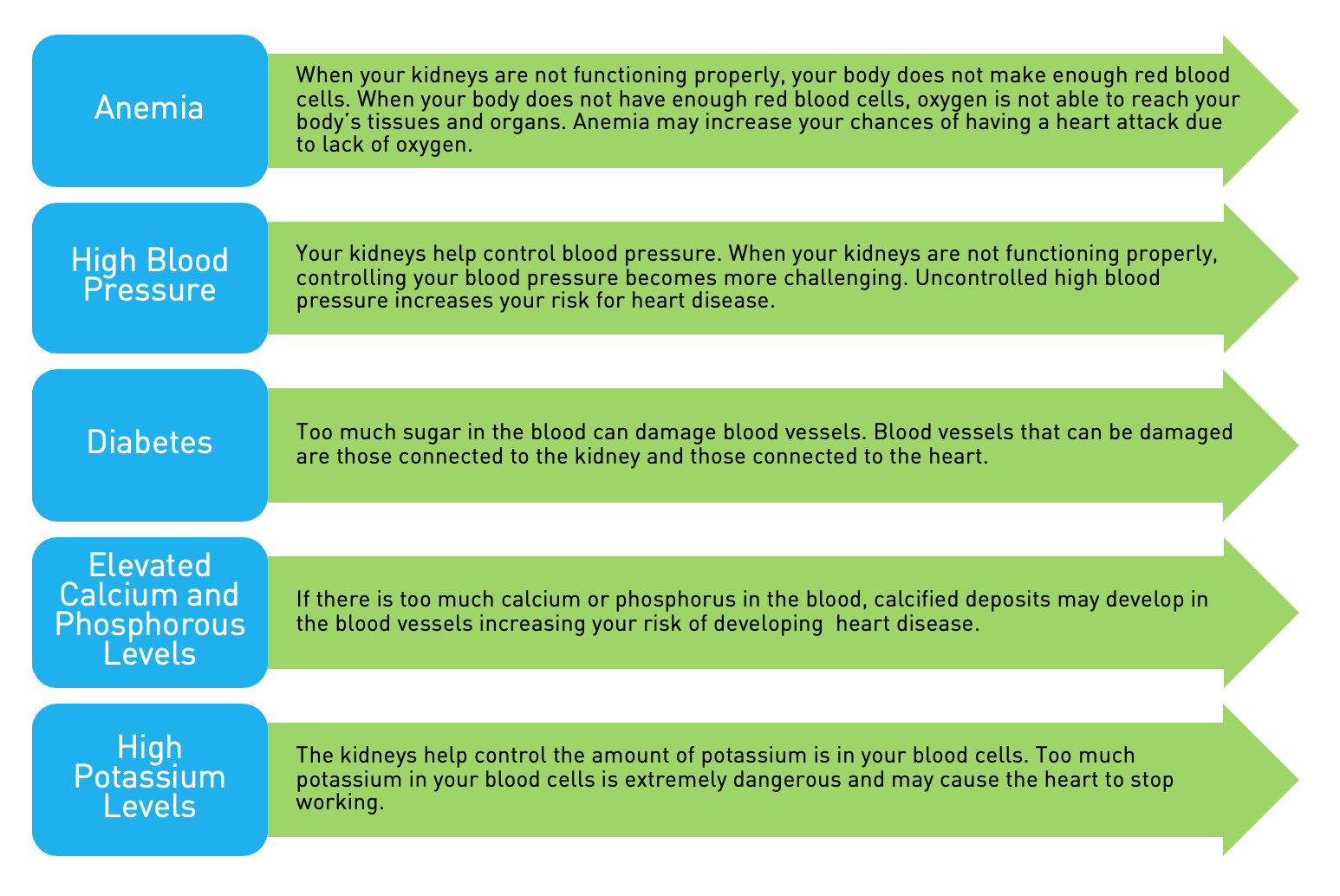
When my kidney function declined to stage 5, I knew it was time to make some very tough decisions. I was a full time mother of three very young children with a promising career in front of me. I struggled to understand how dialysis three times per week away from home would allow me the flexibility and quality of life to maintain adequate balance at work or home? While I firmly believed each patient had different circumstances that dictated their path to continue working, at the age of 27 and with so many aspirations in front of me, drawing disability was not an option. At times my chosen path has been frightening and uncertain, but manageable. My nephrologist shared with me the benefits of shorter, slower treatments which included better blood pressure control, improved energy and (my personal favorite) fewer dietary restrictions. These benefits wouldn’t come easy, but with a lot of determination and family support, I trained for six weeks to learn nocturnal hemodialysis. Once I got the hang of it, I started dialysis six days a week for eight hours a day which eventually turned out to be too much for my body to handle. I was fortunate enough to have a doctor who believed in patient centered care and after reviewing my labs for a three month period, my potassium, phosphorus and BUN stayed chronically low. He adjusted my treatments to eight hours every other day and that’s done the trick for nearly 12 years.
My nephrologist shared with me the benefits of shorter, slower treatments which included better blood pressure control, improved energy and (my personal favorite) fewer dietary restrictions. These benefits wouldn’t come easy, but with a lot of determination and family support, I trained for six weeks to learn nocturnal hemodialysis. Once I got the hang of it, I started dialysis six days a week for eight hours a day which eventually turned out to be too much for my body to handle. I was fortunate enough to have a doctor who believed in patient centered care and after reviewing my labs for a three month period, my potassium, phosphorus and BUN stayed chronically low. He adjusted my treatments to eight hours every other day and that’s done the trick for nearly 12 years.
I’m often asked what it’s like to do my own dialysis along with everything else going on in my life. I’ll share with you a few of my key experiences and responses:
• It’s not easy. At the end of a day filled with work, children’s activities and kidney advocacy – I typically want to simply rest, but my life is not set up that way. My gift of freedom to do those things is earned by setting up my dialysis machine, keeping inventory of supplies, drawing labs, attending monthly doctor’s appointments and dialyzing every other day.
• The alternatives aren’t appealing. I often dialyze in-center across the country when I travel on business and although I’m grateful that option exists, my body does not handle shorter, infrequent dialysis well.
• I’m in charge of my health. Over the years I have learned so much about what my body needs. Even though I have a great medical staff that supports me, I can almost predict what my lab values will be based on how I’m feeling.
You never know where life’s journey will take you. Thinking back on that little girl who thought helping the sick would turn into a career, well she was right. It just happens that the incentives brought about in that career was a daily fight to keep herself alive.
This article was orginally published in aakpRENALIFE, November 2018.