ERA-EDTA Council and the ERACODA Working Group*
Correspondence to: Alberto Ortiz, E-mail: AOrtiz@fjd.es
*A list of members of the ERA-EDTA Council and the ERACODA Working Group can be found as Acknowledgements section.
ABSTRACT
Diabetes, hypertension and cardiovascular disease have been listed as risk factors for severe coronavirus disease 2019 (COVID-19) since the first report of the disease in January 2020. However, this report did not mention chronic kidney disease (CKD) nor did it provide information on the relevance of estimated glomerular filtration rate (eGFR) or albuminuria. As the disease spread across the globe, information on larger populations with greater granularity on risk factors emerged. The recently published OpenSAFELY project analysed factors associated with COVID-19 death in 17 million patients. The picture that arose differs significantly from initial reports. For example, hypertension is not an independent risk factor for COVID-19 death [adjusted hazard ratio (aHR) 0.89], but renal disease very much is. Dialysis (aHR 3.69), organ transplantation (aHR 3.53) and CKD (aHR 2.52 for patients with eGFR <30 mL/min/1.73 m2) represent three of the four comorbidities associated with the highest mortality risk from COVID-19. The risk associated with CKD Stages 4 and 5 is higher than the risk associated with diabetes mellitus (aHR range 1.31–1.95, depending upon glycaemic control) or chronic heart disease (aHR 1.17). In another recent publication, the Global Burden of Disease collaboration identified that worldwide, CKD is the most prevalent risk factor for severe COVID-19. Moreover, the distribution of risk factors for COVID-19 mortality appears to be different in patients with CKD when compared with the general population. The high prevalence of CKD in combination with the elevated risk of mortality from COVID-19 in CKD necessitates urgent action for this group of patients. This article defines essential action points (summarized in Box 1), among which is advocating the inclusion of CKD patients in clinical trials testing the efficacy of drugs and vaccines to prevent severe COVID-19.
Keywords: chronic kidney disease, COVID-19, mortality, prevalence, renal replacement therapy, risk factor
RISK FACTORS FOR SEVERE COVID- 19
By October 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing the coronavirus disease 2019 (COVID-19) pandemic had infected >35 million people with >1 million deaths [1]. An enigmatic and perilous feature of COVID-19 is the wide range of clinical manifestations from asymptomatic to multiorgan failure and death. The high frequency of asymptomatic infection has undoubtedly contributed to the rapid and worldwide spread of SARS-CoV-2 [2]. A key unmet clinical need is the more precise and earlier identification of individuals at high risk of severe disease. These individuals may benefit from shielding and be a priority group for vaccination and for early antiviral therapy before clinical deterioration. Although age is the leading risk factor for severe disease, even the elderly may be asymptomatic or have mild disease. Notably, Spain’s oldest woman, a survivor of the 1918 flu pandemic, survived mild COVID-19 that she probably acquired during her 113th birthday celebrations [3]. The level of exposure to the virus and viral load most likely play a role, as well as poorly characterized genetic and immunological factors. Additionally, several comorbidities are associated with more severe COVID- 19, emphasizing the need to study the disease-associated drivers of the higher risk and the potential impact on COVID-19 of medications commonly used for these diseases. Recently, chronic kidney disease (CKD) emerged as the most common risk factor for severe COVID-19 and alarmingly, after age, is also the strongest risk factor for severe COVID-19 [4, 5].
WHAT IS CKD?
CKD is defined as a decrease in kidney function measured by glomerular filtration rate (GFR) or evidence of kidney damage (even with normal GFR), such as increased albuminuria, abnormal urine sediment or structural abnormalities persisting for >3 months, with implications for health [6]. The GFR and albuminuria thresholds thought to have implications for health are <60 mL/min/1.73 m2 and >30 mg/g of urinary creatinine, respectively. Despite the consensus CKD definition dating back to 2012, there is still insufficient awareness of the concept and a diagnosis of CKD is frequently not recorded in patient medical records [7]. The prevalence of CKD in the adult population has been estimated to be 10–15%, with 850 million people estimated to have CKD globally. CKD is projected to become the fifth leading cause of death by 2040 worldwide and one of the top two causes of death before the end of the century in some European countries, particularly in those countries where life expectancy is longest [8–11]. Indeed, patients with CKD, especially those with kidney failure, are at increased risk of premature death from many causes, including, but not limited to, cardiovascular disease (CVD) and infections [12]. Therapeutic nihilism (e.g. withholding drugs or interventions shown to be effective in the general population) was identified by multiple publications as a potential contributor to the high mortality [12].
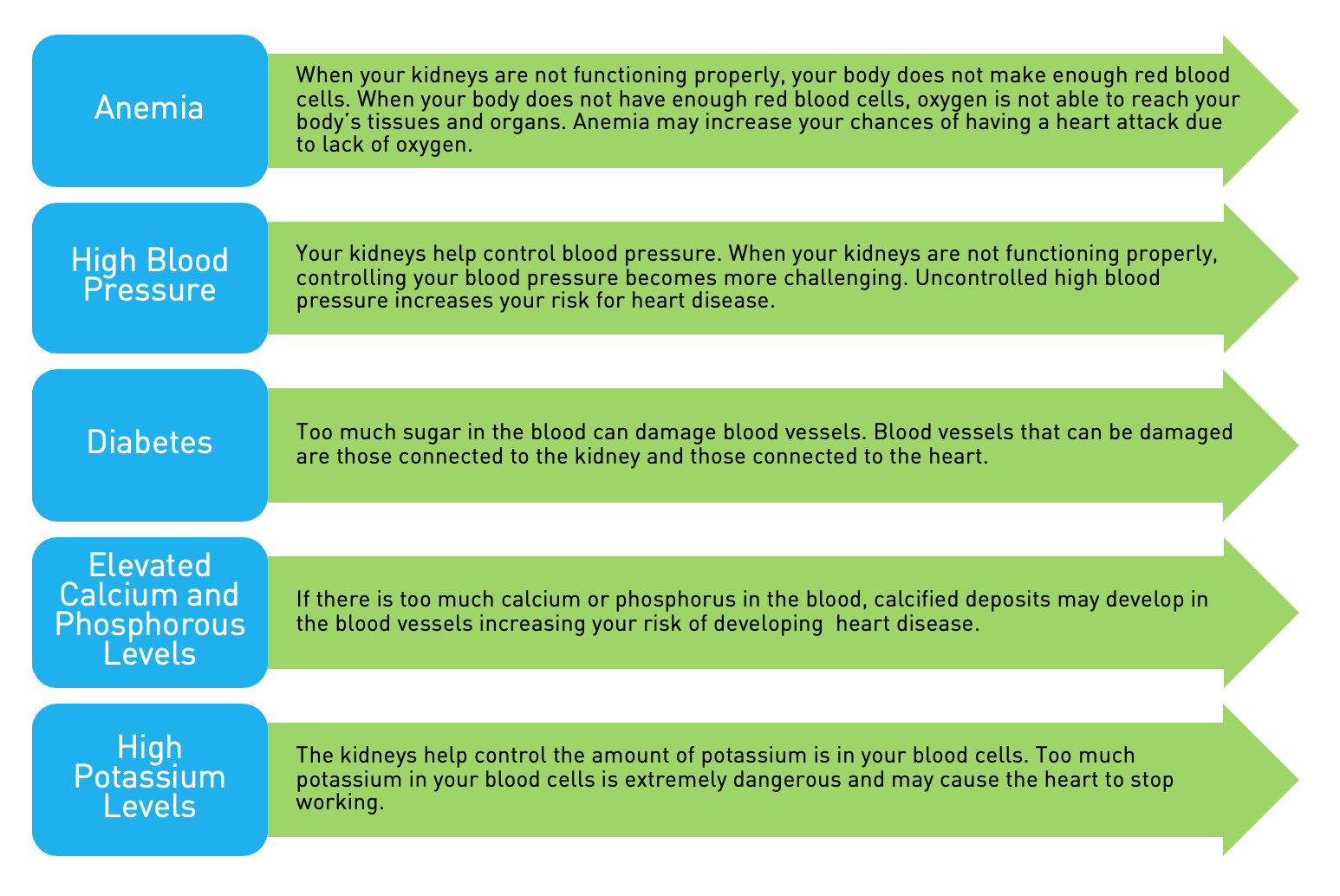
DIABETES, HYPERTENSION AND CVD AS RISK FACTORS FOR SEVE RE COVID–19
The first report of COVID-19 in PubMed is a January 2020 Lancet manuscript describing that among patients admitted with the disease, 20% had diabetes mellitus (DM), 15% hyper- tension and 15% CVD without any information on the prevalence of CKD, estimated GFR (eGFR) or albuminuria [13]. By late March 2020, another report, also from China, listed CKD status, finding it to be a comorbidity in only 1% of 274 COVID-19 patients (median age 62 years), thus likely significantly underreporting the presence of CKD [14]. Chronic hypertension and other cardiovascular comorbidities occurred more frequently among deceased patients. A contemporary systematic review and meta-analysis of 76 993 patients presented in 10 articles listed CKD among the seven most prevalent coexisting diseases (alongside hypertension, CVD and DM) among hospitalized COVID-19 patients [15]. Another meta- analysis of four studies including 1389 COVID-19 patients noted that although no study individually found CKD to be significantly associated with severe COVID-19, in the combined analysis CKD was linked with severe COVID-19, without relevant heterogeneity odds ratio 3.03 [95% confidence interval (CI) 1.09–8.47], I 0.0%, Cochran’s Q, P 0.84 [16].
Furthermore, in March 2020, UK political and health authorities advised vulnerable persons, including those with CKD, to ‘shield’ (i.e. minimize their social contacts) [17]. This statement drew criticism for not considering the fact that CKD can vary from mild to severe and that this could have consequences [18]. Thus early reports failed to adequately assess the prevalence of CKD and to gauge its impact on COVID-19 disease severity and instead focused on CKD-associated conditions (e.g. hypertension and DM). This is despite acknowledgement of CKD as a known risk factor for severity of several other bacterial and viral infections. As early as the end of March, some authors were calling for CKD to be recognized as a high- risk condition. Half a year later, in September 2020, a PubMed search for CKD and COVID-19 yielded >314 results and it has been found CKD is a key risk factor for severe COVID-19.
CKD IS THE MOST PREVALENT RISK FACTOR FOR SEVERE COVID-19 WORLDWIDE
The Global Burden of Disease (GBD) collaboration, which provides information on the health of populations worldwide annually, recently addressed the prevalence of risk factors for severe COVID-19 worldwide [5, 18]. The GBD produces age-, sex- and country-specific health estimates using highly standardized, validated approaches applied to all available data sources and adjusting for major sources of bias. Using 2017 prevalence data and UN population estimates for 2020, the GBD estimated the number of individuals at increased risk of severe COVID-19 by age, sex and country for 188 countries. This study estimated the global population at high risk for severe COVID-19 to be 1.7 billion people, comprising 22% of the global population, of whom 349 million would require hospital admission if infected. CKD was the most prevalent risk factor for severe COVID-19 worldwide [5]. It was the most common risk factor and as frequent as CVD at any age (Figure 1). Removal of CKD as a risk factor would decrease the percentage of the global population at increased risk of severe COVID-19 from 22% to 17%. Thus CKD explains the increased risk of severe COVID-19 for about one in four high-risk individuals worldwide (Supplementary data, Figure S1), equivalent to 5% of the global population, or 86 530 000 persons.
CKD IS THE DISEASE CONDITION CONVEYING THE HIGHEST RISK FOR SEVERE COVID-19
Williamson et al. [4] recently published the largest analysis to date of risk factors for severe COVID-19 resulting in death. They analysed data from >17 million adults with almost 11 000 COVID-19-related deaths using OpenSAFELY, a health analytics platform that covers 40% of all patients in England. In the abstract, the authors state that COVID-19-related death was associated with male sex [adjusted hazard ratio (aHR) 1.59 (95% CI 1.53–1.65)], older age, deprivation, DM, severe asthma, Black and South Asian ethnicity and ‘various other medical conditions’. CKD is not mentioned in the abstract, yet from the full paper it is clear that advanced CKD (categories G4 and G5) was among the conditions conveying the highest risk of death and notably higher than that conferred by all other factors mentioned in the abstract. Indeed, in a fully adjusted model including adjustment for age, patients with kidney disease, for ex- ample dialysis patients (aHR 3.69), transplant recipients (aHR
3.53) and CKD (aHR 2.52 for patients with eGFR <30 mL/min/1.73 m2, CKD G4–G5), represented three of the top four risk categories. The risks in these subgroups were greater than the risk for COVID-19 death in diabetic patients (aHR range 1.31–1.95, depending upon glycaemic control) and in patients with chronic heart disease (aHR 1.17) (Figure 2). In sensitivity analyses with different populations [early censoring, restricted to those with complete body mass index (BMI)/smoking data, adjusted for recorded or imputed ethnicity], the risk conferred by CKD G4–G5 was consistently higher than the risk conveyed by poorly controlled DM or severe asthma, which makes it all the more puzzling that CKD was not among the risk factors detailed in the abstract.
Data for hypertension are interesting. Despite having been widely mentioned as a risk factor for severe COVID-19, in an analysis adjusted for age and sex it was only weakly associated with the risk of death [HR 1.09 (95% CI 1.05–1.14)]. In a fully adjusted analysis, the risk associated with hypertension was in fact reversed [aHR 0.89 (95% CI 0.85–0.93)], thus suggesting that hypertension may be a surrogate for other conditions (e.g. CKD) that convey the risk. A further explanation might be that the risk associated with hypertension is influenced by the use of certain drugs [e.g. renin–angiotensin system (RAS) blockers]. Although initially hypothesized that RAS blockade may in- crease the risk of severe COVID-19 by increasing angiotensin- converting enzyme 2 expression (and subsequent virus entry into cells) or decrease the risk of severe COVID-19 by promoting angiotensin(1-7) synthesis, neither of these hypotheses has been proven thus far in epidemiological studies, which instead tend to show a neutral effect [18, 19]. The potential impact of RAS blockade was not assessed in OpenSAFELY. Ultimately, even when CKD is clearly demonstrated to be among comorbidities that convey the highest risk of death in COVID- 19, it is replaced in the article ‘headline’ (i.e. the abstract) by more ‘popular’ conditions that somewhat ironically are actually associated with a lower COVID-19 mortality risk than CKD.
In a separate UK population-based cohort study undertaken in a general practice context, age and eGFR were the variables that most strongly affected the aHRs for COVID-19-related death in people with type 1 (T1DM; n 264 390) and type 2 di- abetes (T2DM; n 2 874 020) (Figure 3) [21]. The increased risk was evident from eGFR 45–59 mL/min/1.73 m2, but not with an eGFR above that value, in both T1DM and T2DM, i.e. it was evident for patients with CKD as defined by eGFR thresholds. Unfortunately, similar to the OpenSAFELY study, the effect of increased albuminuria was not analysed. Thus the increased risk of persons with CKD G3–G5 was confirmed, but information on CKD G1–G2 was lacking, as in other epidemiological studies. Of the different variables analysed, an eGFR<15 mL/min/1.73 m2 conferred the highest risk of death after age, both in T1DM [aHR compared with eGFR 90 mL/min/1.73 m2 8.35 (95% CI 5.50–12.70)] and in T2DM [aHR 4.91 (95% CI 4.34–5.56)]. Other variables analysed included sex, socio-economic status or deprivation, ethnicity, haemoglobin A1c, BMI, blood pressure, antihypertensive drugs, smoking status and cardiovascular comorbidities. HRs for impaired kidney function were consistent for males and females and were greater for people <70 years of age.
Results from the ERA-EDTA Registry further support the high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe [22]. The 28-day mortality was 20.0% (95% CI 18.7–21.4%) in 3285 patients receiving dialysis and 19.9% (17.5–22.5%) in 1013 recipients of a kidney transplant. Mortality risk was 1.28 (95% CI 1.02–1.60) times higher in transplant recipients compared with age- and sex- matched dialysis patients. In both groups, mortality is in large part related to age and in dialysis patients also to frailty status [23]. In addition, frequent hospital attendance, as is needed for in-centre dialysis, may increase the risk of infection for end- stage kidney disease patients [24].
A missing piece of information is quantification of the risk con- veyed by pathological albuminuria. This may be the sole criterion that defines CKD when eGFR is 60 mL/min/1.73 m2 or may fur- ther increase risk in CKD patients with a lower eGFR. Interestingly, COVID-19 itself may result in glomerular injury, evidenced by the occurrence of proteinuria, which can be associated with acute kid- ney injury [25]. In turn, acute kidney injury can lead to CKD, and when superimposed on CKD, it increases the risk for mortality con- veyed by CKD even further [26, 27]. These data also indicate that SARS-CoV-2 has multiorgan tropism that includes glomerular and, as was later shown, tubular cells [28, 29].
END-STAGE KIDNEY DISEASE AND THE NEED FOR SPECIFIC STUDIES
Emerging data revealed risk factors for severe COVID-19 among patients on kidney replacement therapy. The European Renal Association COVID-19 Database (ERACODA) cohort, established by the ERA-EDTA, showed that within dialysis and kidney transplant populations the risk conferred by classical risk factors for severe COVID-19 is completely different than in the general population [23]. For instance, in dialysis patients with COVID-19 [n 768, of which 192 (25%) died], the relative contribution of age to mortality is considerably less than in subjects from the general population. In addition, in dialysis [22, 23]; given the discrepancies between risk factors in this population as compared with the general population [23], findings in the general population cannot and should not be extrapolated to end-stage kidney disease populations. There are other compelling reasons why the CKD population merits specific study. During the last 2 decades it has become clear that some drugs that are effective in patients with normal kidney function have little or no efficacy in patients with impaired kidney function, especially in those on dialysis. This holds true for, among others, statins [30]. Medications prescribed to lower COVID-19 morbidity and mortality must therefore be tested in patients with impaired kidney function to prove their efficacy in this patient category. Unfortunately, randomized clinical trials often exclude patients with impaired kidney function due to safety reasons [10]. It is our recommendation that the kidney community should take great care to include CKD patients in COVID-19 medication trials to avoid dis- parities in the treatment of this patient group. A first step in achieving this is propagating awareness of the importance of CKD as a key risk factor among the general com- munity and policymakers so that the problem is recognized. Furthermore, we know that because of the immunosuppressive nature of the uraemic milieu in dialysis patients and because of the use of immunosuppressants in transplantation patients, these patients respond poorly to vaccination [31]. It is therefore imperative that CKD patients be included in trials testing the efficacy of vaccines against SARS-CoV-2 infection. It is very plausible that in such patients different vaccination schedules may be necessary (e.g. a higher dose or repeat vaccinations).
CONCLUSIONS
Although not listed in initial reports as a risk factor for severe COVID-19, CKD has emerged not only as the most prevalent comorbidity conveying an increased risk for severe COVID-19, but also as the comorbidity that conveys the highest risk for severe COVID-19. The increased risk is evident below the thresh- old of eGFR that defines CKD and the risk increases as the eGFR decreases, with the highest risk in patients on kidney re- placement therapy. Although CKD patients are known to be at increased risk of death due to infectious diseases, the factors contributing to their greater vulnerability for severe COVID-19 should be explored, as these may provide valuable insights into therapeutic approaches to the disease in this patient group. It is presently unknown if earlier categories of CKD (G1/G2, i.e. patients with preserved kidney function but with increased albuminuria) are also at an increased risk of severe COVID-19, and this must be explored. Moreover, the recognition that CKD significantly contributes to the severity of COVID-19 should now result in focused efforts to improve outcomes for the 850 million global CKD patients [8]. Paramount to this is the enrolment of patients representing all CKD stages, including dialysis and transplantation, in clinical trials of vaccines to prevent and drugs to treat COVID-19.
Crucially, a CKD diagnosis should not be used as the sole criterion to deny intensive care admission with severe COVID-19. Both scientific societies and patient associations should be vigilant in this regard. Until better epidemiological data become available and the biological basis of the increased risk of severe COVID-19 in CKD patients is ascertained, therapeutic nihilism may continue to play a role and CKD patients may be denied vital support based on their increased risk of COVID-19-related death. This becomes an unacceptable self-fulfilling prophecy. The threatening shortage of intensive care unit capacity in some parts of the world may have contributed to the high mortality of CKD patients in these areas. In those with kidney disease, therapeutic nihilism has been repeatedly associated with ad- verse outcomes [11]. Facing an ongoing pandemic of unquantifiable duration, this is not an acceptable strategy, particularly considering the high prevalence of CKD. We propose that those with CKD must be actively included in research to ensure equitable access to effective vaccines and treatments in the future.