Download the Official Letter (link to attached PDF)
June 16, 2020
Shannon Lee
Centers for Disease Control and Prevention (CDC) 1600 Clifton Road NE, Mailstop S106-9
Atlanta, GA 30329
Re: Docket No. CDC-2020-0029
Dear Ms. Lee:
On behalf of the undersigned members of the Protecting Access to Pain Relief (PAPR) Coalition, please find written comments in response to the Request for Comment entitled “Management of Acute and Chronic Pain” (Docket No. CDC-2020-0029) issued by the Centers for Disease Control and Prevention (CDC). We appreciate the agency’s efforts to obtain additional information related to patient, provider, and caregiver experiences with pain and pain management, which may help inform the agency’s educational efforts on these issues, especially in helping to educate these populations about the importance of non-opioid alternatives to pain management.
The PAPR Coalition is a multi-stakeholder group of public health organizations whose mission is to support continued access to and choice of appropriate over-the-counter (OTC) pain relief, including acetaminophen, as part of a patient’s comprehensive pain management plan, including for use as alternatives to opioids (www.paprcoalition.com). Collectively, our Coalition reaches millions of healthcare professionals, people living with pain, patients managing chronic disease, and concerned citizens. Our combined communications and engagement platforms have proven to be a powerful resource with the demonstrated capacity to educate and mobilize Americans on complex and timely public health issues. The Coalition is strongly supportive of efforts to increase knowledge and resources around pain management for Americans across the life course, including through developing comprehensive graduate medical education on pain management, encouraging the development of a multi-disciplinary approach to pain management utilizing non- opioid alternatives where appropriate, expanding payment schemes to improve access to appropriate pain management options, increasing research into novel pain management practices, and encouraging additional federal coordination on pain management policies.
Currently, chronic pain affects an estimated 50 million U.S. adults, and as many as 19.6 million of those adults experience high-impact chronic pain that interferes with daily life or work
activities.1 Because of its near ubiquity nationwide, pain presents a significant public health problem in the U.S. An Institute of Medicine report found that pain costs our society at least $560-$635 billion annually (equal to about $2,000 per person) in lost wages and compensation for disability days.2 In addition, the costs of care associated with chronic pain, which include diagnostic tests, physical therapy, medications, and medication management, can be extremely burdensome on both patients and the healthcare system as a whole. A 2015 study of a large U.S. health integrated delivery system indicated that treating chronic pain costs approximately
$32,000 per patient per year, with an annual average of nearly 19 outpatient visits and five imaging tests per patient.3
We agree with the statement by Department of Health and Human Services (HHS) Secretary Alex Azar and Assistant Secretary Adm. Brett Giroir that “[A]s we combat the opioid crisis, we cannot forget that pain is a real problem…We must do a better job of securing for them safe, effective options for managing pain.”4 Recent research has shown that non-opioid pharmacologic alternatives have been shown to be as effective, if not more effective, than opioids in treating chronic pain over time.5 The Coalition believes policy makers should take additional steps to educate healthcare providers and patients about the important role of OTC pain medication as part of a safe and responsible pain management plan.
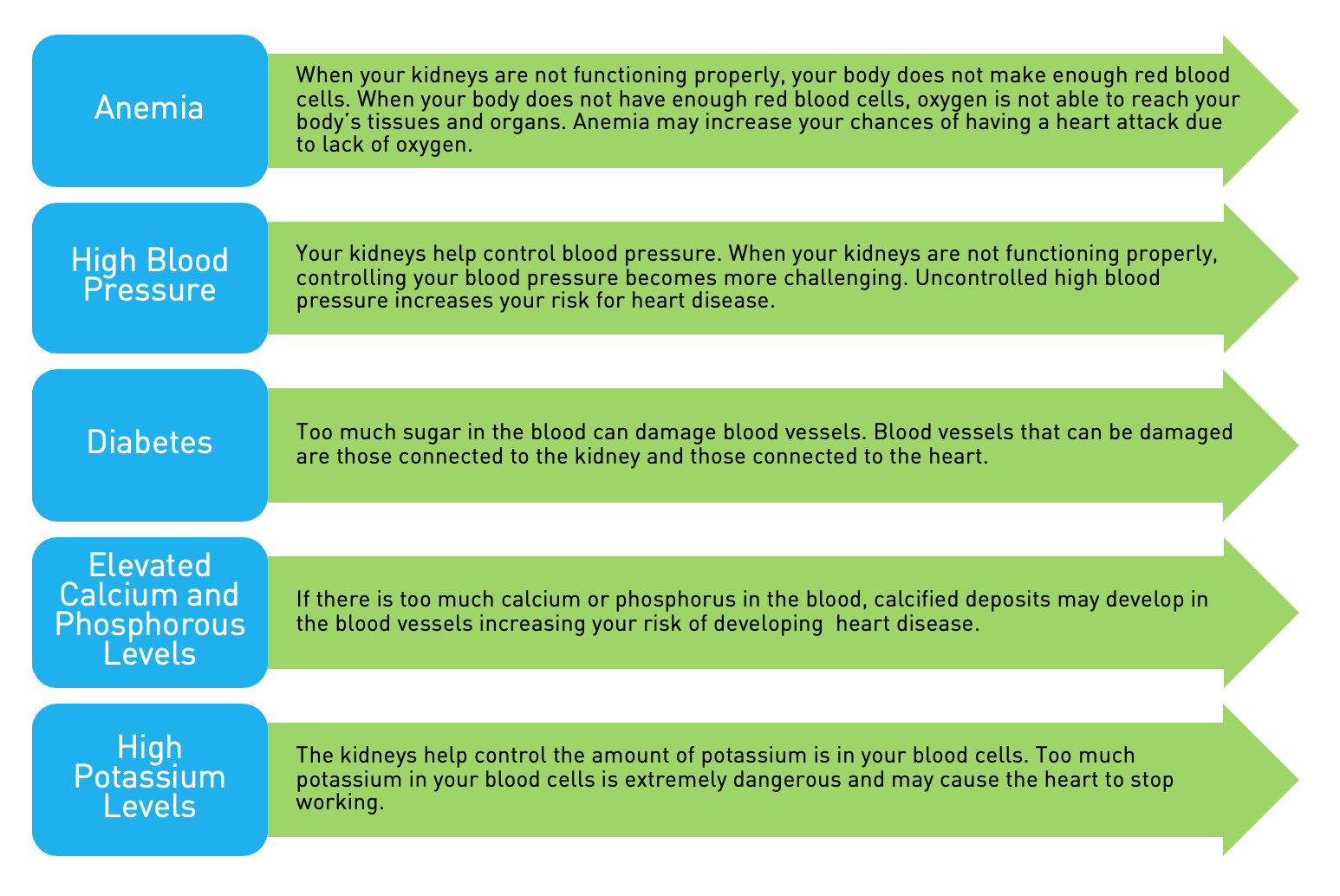
OTC pain relief – including use of acetaminophen – is often a medically necessary and cost effective way for patients to manage pain. In addition to lower costs, for many older adult patients, such as those suffering from osteoporosis and end stage renal disease, OTC pain relief represents the safest medically recommended means of alleviating pain. It is important for Americans to have access to and choice of the appropriate OTC pain relief to match their pain profile and comorbidities and to offer safe and effective alternatives to the use of opioids where opioids may be inappropriate or contraindicated for particular conditions.
Indeed, the Coalition appreciated the CDC’s efforts in 2016 to update its guidelines to indicate that opioids should no longer be considered the first-line treatment option for noncancer pain.6 Recent research from multiple national organizations has also indicated the increased adoption of multimodal pain management regimens that utilize OTC analgesics due to their positive balance Protecting Access to Pain Relief (PAPR) Coalition, please find written comments in response to the Request for Comment entitled “Management of Acute and Chronic Pain”between patient safety and efficacy.7 Finally, studies have indicated that opioids are no more effective for improving long-term, pain-related functions. For instance, one study determined that treatment with opioids was not superior to treatment with OTC analgesics for moderate to severe chronic back pain or hip/knee osteoarthritis pain.8
Given these facts, the PAPR Coalition strongly supports the use of OTC and other non-opioid alternatives for the appropriate treatment of pain across the lifespan. For example, it is important that a multidisciplinary approach that utilizes non-opioid alternatives such as OTC analgesics be utilized in the adult population over the age of 65. The use of non-opioid alternatives in this population expands access and lowers barriers to safe and effective pain relief by potentially reducing office visits in between regular and necessary evaluations. This point is especially important as older populations and those with lower mobility seek treatment during the COVID- 19 pandemic. The use of non-opioid alternatives is also important for this population whose members are frequently more susceptible to both respiratory depression and reduced medication clearance related to decreased renal function.9
Issues of pain management and opioid use and misuse extend beyond adult and older populations to youth and adolescents, as well. Communications and policies should be designed with these populations in mind. The PAPR Coalition supports the use of OTC analgesics for the treatment of chronic pain in the pediatric population, especially as a pain relief alternative for the 3.1 percent of youth ages 12 to 17 and 7.3 percent of adolescents ages 18 to 25 that reported misusing opioids.10 Given the propensity for behaviors developed in childhood to continue into adulthood, non-addictive pain relief options, such as OTC analgesics, represent safe and effective alternatives to help prevent future opioid misuse. Further, the Coalition urges parents and caretakers to carefully follow the advice of their provider in providing OTC medicines to children and to follow any evidence-based and scientifically valid weight-based dosing information for these populations. The Coalition is currently working with policymakers to ensure that weight-based dosing information for children ages six months to two years is applied to acetaminophen labeling to promote safe administration of these products to children.
The PAPR Coalition also encourages CDC and others to collect and disseminate data regarding chronic pain in patients so that specific resources may be developed that are targeted to special populations suffering from non-neuropathic, non-cancer pain. This includes making investments in additional research to generate data on novel pain management options. For instance, there have been recent calls for data and research on new approaches combining both pharmacologic and non-pharmacologic – rehabilitation or exercise – pain management interventions that could be successful in managing pain, including and especially in older or less mobile populations.11 In fact, past studies have indicated that physical therapy can be as effective in reducing symptoms, such as pain, and improving mobility as surgical interventions.12 Additional research in this and other promising approaches, including approaches such as exercise that were highlighted by the CDC’s 2016 guidelines, is needed to inform guidelines that are easily interpreted by young and old populations alike and allow for adaptation over time as the American healthcare system changes, including and most recently with the uptake of telehealth as a means to further novel pain management.13 Safe and effective alternative methods for pain management should be accompanied by payment schemes that increase access to safe and effective pain management alternatives, especially structures that promote equity for coverage of non-opioid alternatives to pain relief for the patients that need them. This includes coverage options that maximize the ability of physicians and non-physicians providers, such as nurse practitioners, physician assistants, pharmacists, etc., to provide comprehensive pain management to the patients that need them and for out-of-pocket expense for the patient to be negligible or free.
One of the main tenets of the PAPR Coalition’s mission is to educate patients about the safe use of OTC pain relief options, especially as an alternative to opioids. In pursuit of this goal, the Coalition developed and submitted an application in 2017 under the Food and Drug Administration (FDA)’s Safe Use Initiative. By utilizing the expertise of the its collective membership, the Coalition developed a proposal to test the impact of behavioral economics- based digital messaging campaigns to educate patients about the safe use of acetaminophen. In its response to the Coalition’s Safe Use Initiative application, the FDA indicated that “the prevalence of unintended acetaminophen overdose is very low; 200 per year [in the United States].” While a positive indicator that current educational tools, labeling, and other forms of public information are working to help protect patients from unintentional harm, the Coalition will continue to promote a diverse array of educational materials on this issue.
Collectively, the Coalition is able to reach and disseminate educational materials to millions of patients, their families, caregivers, and health care providers. The Coalition will continue to serve as a resource for patients suffering from chronic pain, and encourages the CDC to work collaboratively with the Coalition, its members, and other external stakeholders to cross- promote, develop, and disseminate educational materials for the benefit of patients across the nation. In addition, the Coalition’s members have strong relationships with scientific experts, patients, and advocates that can be useful for the creation of expert panels related to pain management and education. This CDC request for comment is an important step to ensuring that the patient voice is heard and incorporated into effective educational materials that can help promote safe and effective pain management.
Finally, it should be noted that the patient voice should also be incorporated into the expansion of pain management education for providers. Comprehensive training in the development and execution of pain management plans for patients is frequently left out of graduate medical education curricula and current practice.14 In large part, these issues stem from inconsistent and disparate federal guidelines for pain management despite a large body of evidence that can inform a series universal best practices within the U.S. healthcare system. The incorporation of the patient voice and experience into these educational efforts is important for greater understanding by the medical community about the most productive and appropriate manner for treating a patient’s pain. This information can be incorporated into training, to include specific residency programs, internships, and other resources, not only for physicians but also for the full range of healthcare providers, such as nurse practitioners, physician assistants, and pharmacists, who are intimately involved with care coordination, and treatment determination, for patients with pain management needs.
Thank you again for your interest in these issues and for initiating this request. Insights from patients, providers, and caregivers are extremely important for the development of any guidelines or policies to inform national pain management practices as well as opportunities for education on the importance of non-opioid alternatives for pain management. The PAPR Coalition and its members look forward to serving as a resource to the agency in its efforts to address issues
related to the safe and appropriate management of Americans’ pain.
Should you have any questions regarding this submission, please contact Michael Werner (michael.werner@hklaw.com) and Joel Roberson (joel.roberson@hklaw.com).
Sincerely,
Alliance for Aging Research
American Academy of Pediatric Dentistry American Association of Kidney Patients American Gastroenterological Association American Pharmacists Association American Society of Nephrology BeMedWise Program at NeedyMeds
The Gerontological Society of America National Minority Quality Forum Renal Physicians Association TransplantFirst Academy
Veterans Transplantation Association
1 Dahlhamer J. et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults – United States, 2016. Morbidity and Mortality Weekly Report (MMWR). 2018; 67(36):1001-1006.
2 Institute of Medicine Report from the Committee on Advancing Pain Research, Care, and Education: Relieving Pain in America, A Blueprint for Transforming Prevention, Care, Education and Research. The National Academies Press, 2011.
3 Park PW et al. Cost burden of chronic pain patients in a large integrated delivery system in the United States. Pain Practice. November 2016; 16(8):1001-1011.
4 Azar A and BP Giroir. While fighting the opioid epidemic, don’t forget those who are suffering from pain. Department of Health and Human Services. 1 June 2018. https://www.hhs.gov/blog/2018/06/01/dont-forget-those- who-are-suffering-from-pain.html.
5 Krebs EE et al. Effect opioid vs. nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. Journal of the American Medical Association. 2018; 319(9):872-882.
6 Dowell D et al. CDC Guidelines for Prescribing Opioids for Chronic Pain – United States, 2016. Morbidity and Mortality Weekly Report (MMWR). 18 March 2016; 65(1):1-49.
7 Nalamachu S. et al. Over-the-counter analgesics for the management of acute pain: Clinical experience in the era of the opioid crisis. Pain Management News (supplement). January 2019. https://www.painmedicinenews.com/download/SR194_WM.pdf.
8 Krebs EE et al. Effect opioid vs. nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. Journal of the American Medical Association. 2018; 319(9):872-882.
9 Wu A. Special consideration for opioid use in elderly patients with chronic pain. U.S. Pharmacist. 16 March 2018; 43(3):26-30.
10 Substance Abuse and Mental Health Services Administration (SAMHSA) (2017) Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52) Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www. samhsa.gov/data/.
11 Federal Pain Research Strategy. Interagency Pain Research Coordinating Committee. National Institutes of Health. 12 Dec. 2018. https://www.iprcc.nih.gov/sites/default/files/iprcc/FPRS_Research_Recommendations_Final_508C.pdf.
12 Delitto A et al. Surgery versus nonsurgical treatment for lumbar spinal stenosis: A comparative effectiveness randomized trial with a 2-year follow-up. Annals of Internal Medicine. 7 April 2015; 162(7):465-473.
13 Dowell D et al. CDC Guidelines for Prescribing Opioids for Chronic Pain – United States, 2016. Morbidity and Mortality Weekly Report (MMWR). 18 March 2016; 65(1):1-49.
14 Mezei L and BB Murinson. Pain education in North American medical schools. J Pain. December 2011; 12(12):1199-1208.