By Stephen Z. Fadem, MD, FASN, AAKP Medical Advisory Board Chair, and Michelle (Misha) L. Nguyen, Senior Fitness Specialist
February was rodeo season in my hometown of Houston, Texas. Here is where young cowboys compete to stay on a 2,000-pound snorting, ornery, bucking, kicking, and twisting bull for
at least eight seconds. The only thing for certain is that the cowboy will inevitably fall off. Bull riders prepare extensively for their eight seconds of exhilaration and treacherous dismount. They wear protective vests, mouthguards, and helmets. They exercise, stay fit, study how to land on their hands and feet, then run for their lives to the nearest gate. With a 100% certainty that one will fall, preparation becomes essential. But what if the certainty of falling is 33 to 35%, such as in the elderly [1]? In 90-year-olds, the risk rises even higher; 58% are reported to fall once a year [2]. While bull riders have a 3.2% injury rate [3], hemodialysis patients who fall have over twice the incidence of sustaining a head injury at 7%. Fractures are a consequence of falls and, according to the World Health Organization (WHO), the cause of over 50% of accidental injury, and 39% of fatal injury in the elderly population [4]. This well encompasses those with kidney disease. Falls are the fifth leading cause of death in the general population. Once a person has fallen, the risk for subsequent recurrent falls increases even further.

Given the odds of falling and the unfortunate potential for an adverse consequence, it is imperative that individuals with chronic kidney disease (CKD), especially the elderly with this condition, are aware of fall risks, prepare accordingly, and remain vigilant to the negative consequences in order to avoid falls.
Fall Categories
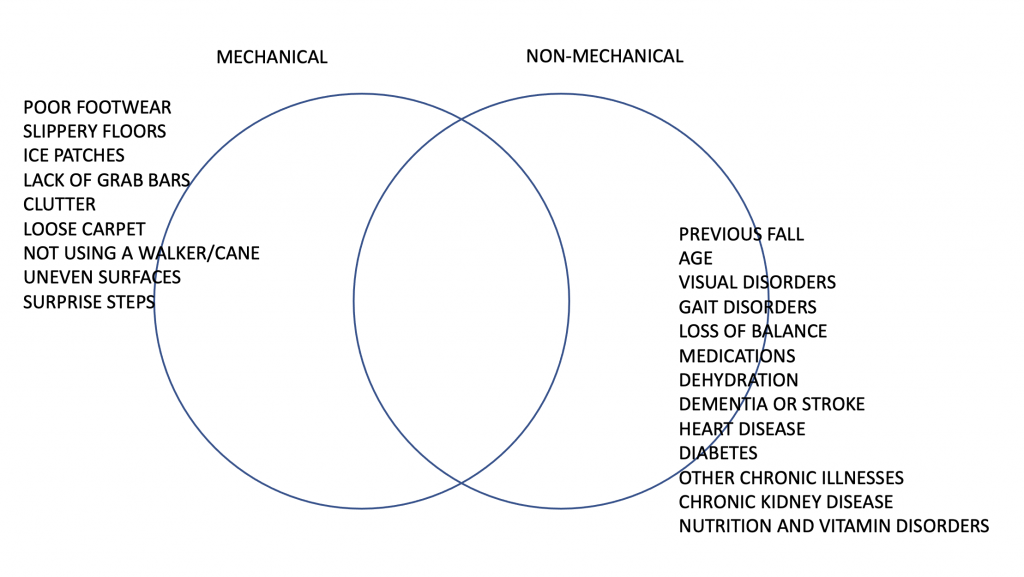
Falls can be divided into two categories–mechanical and non-mechanical. Mechanical falls, i.e., slips and trips, are caused by environmental factors such as poor lighting, clutter, slippery floors, or obstacles on the floor. Falls can also be the result of underlying diseases and conditions. Age and living alone are both risk factors of falls, as well as vision impairment, improper footwear, or underlying gait (walking) disorders. Seemingly minor foot problems such as bunions or ulcers can also lead to unsteadiness and falls. As we age, we tend to lose our sense of balance, which may also result in falls. Arthritis, especially in the knees, may be associated with muscle and bone weakness, pain, and unsteadiness. This is compounded with other disorders such as high blood pressure, heart disease, diabetes, or CKD. Medications most commonly linked to falls include the excessive use of sedatives or drugs used to treat blood pressure or diabetes. Cardiovascular disease can result in a fall as a consequence of a sudden arrhythmia (heart rhythm disturbance). Dehydration, the result of poor fluid intake, vomiting, or diarrhea, can also lead to a fall. Medical conditions such as stroke or dementia can also increase the risk of falls. Diabetes is not only associated with the potential for hypoglycemia, but a neurological condition known as autonomic insufficiency. This causes postural hypotension. Kidney disease has its own set of risks–metabolic acidosis and disorders of mineral metabolism–which result in the loss of bone mass. Abnormal vitamin D metabolism can impair the formation of new bone, while an inherent excessive production of parathyroid hormone by tiny glands located in the neck increases bone disintegration and breakdown. This makes bones more fragile, increasing the risk for a fracture. Kidney disease directly leads to muscle loss, also called sarcopenia[5]. In advanced CKD, as well as metabolic acidosis and sedentary behavior, muscle cells are targeted and tagged for breakdown and recycling. Sedentary behavior may occur with advancing age, underlying conditions such as CKD, or even a fear of falling. Not just decreased activity, but a lack of exercise also promotes muscle loss. In the average person, muscle breakdown can occur at 1% per year, but this is exaggerated in CKD. Sarcopenia has been associated with mortality, functional decline, and a high risk of falls[6].
Preventing Non-Mechanical Falls
Efforts should be made to prevent falls whenever possible. There is considerable overlap between mechanical and non-mechanical falls. In other words, patients who are at higher risk for falls because of an underlying condition are also more likely to sustain a mechanical fall.
Both mechanical and non-mechanical risk factors should be evaluated for each individual to make management and prevention decisions that can help avoid falls. The most important risk factor is a previous fall. Risks can be further evaluated by assessing one’s gait, muscle strength, and ability to hold one’s balance. It is further assessed by identifying visual acuity disorders such as cataracts, macular degeneration, glaucoma, or the need to adjust the corrective lens. Assessing footwear and inspecting the feet for non-healing diabetic ulcers, the loss of pain sensation, or bunions is likewise important.
t is essential to optimize care for most underlying conditions by consulting with your doctor and reviewing medications at each visit. Excessively controlled diabetes is associated with hypoglycemia. When overmedicated with antihypertensives, one can become dizzy upon standing and easily fall. Sedatives and pain medications may lead to drowsiness and result in a fall. Vitamin D deficiency is associated with falls and can be remedied with the use of supplements.
Hemodialysis puts patients at high risk for a fall, particularly at the end of their treatment, when dialysis fluid removal has resulted in a large volume shift. Many patients with ESKD (end-stage kidney disease) also have underlying hypertension and heart disease. Therefore, they are on blood pressure-lowering medications and, if diabetic, may also have neuropathy. The blood pressure tone that normally compensates for a shift in volume is absent, particularly in patients with advanced diabetes. The excess removal of fluids may cause the blood pressure to be low as the treatment ends because there is no mechanism to enable compensation. Combining these factors increases the chance of losing one’s balance and falling. Dialysis personnel are well aware of this phenomenon and often accompany high-risk dialysis patients to the waiting room after their treatment.
Preventing Mechanical Falls
If at risk for a fall, one should seek medical care to stabilize underlying clinical conditions such as heart failure, diabetes, or kidney disease. This may include working with a physical therapist to treat gait disturbances, getting one’s vision evaluated, and visiting an ophthalmologist. Medications causing low blood pressure, low blood sugar, or leading to oversedation should be minimized. One should review his or her medications routinely with a provider and see an orthopedist or foot specialist to determine if footwear is proper and if there are any disorders that could result in a fall.
One should also fall-proof his or her living quarters. This includes inserting grab bars in the bathroom and shower areas to prevent slipping. Carpeting should be secure, slip-resistant, and padded. Those with gait disturbances, dementia, or balance disorders should have assistance when walking on uneven surfaces or approaching small “surprise” steps. Nightlights are inexpensive yet essential, as well as the practice of making sure anything that could clutter a pathway has been safety removed prior to going to bed. Stairs should always have handrails, and those at risk should never climb up or down the staircase without using them.
Many people who are at risk of falling are fearful of increasing activity. This can lead to further danger because inactivity weakens both bones and muscles. However, activity should be planned with caution and, if necessary, assistance should be provided. Physical therapy might be useful for those with a physical impairment. For many individuals, a personal trainer, particularly a certified senior fitness specialist, can offer invaluable tips for seniors on how to increase or maintain activity safely.
Individuals with kidney disease are often on multiple medications and at risk for fractures, loss of balance, and cardiac disturbances. The patient with advanced kidney disease, like the elderly patient, should be treated with vigilance.
Elastic bands are inexpensive and can be used for various resistance training exercises. The photo shown to the left is a demonstration of the biceps curl. Stand with feet at shoulder length apart and straddle the band. Perform a full curl by flexing the biceps (upper arm motion) and then releasing back to starting position 10 to 15 times. Repeat for a total of three sets.
Even if one is not a direct risk for falling, many of the steps above help to improve one’s well-being. There are several exercises one can do to increase strength and improve balance. Resistance training helps offset the muscle loss associated with kidney disease and aging. Balance exercises can build back muscle memory and improve one’s equilibrium. Many practical exercises are discussed in “Staying Healthy with Kidney Disease.” These exercises are highlighted by Senior Fitness Specialist Michelle (Misha) L. Nguyen to help improve balance and preserve muscle[7, 8]. Exercise has been demonstrated in a large systemic review to reduce falls in community environments[9]. Tai chi classes can improve balance. Walking up the stairs can build up the muscles in the back of the leg and the gluteus area, while walking down the stairs can help rebuild and strengthen bone. Always use the handrail. In addition, all patients should try to learn how to land safely to prevent serious injury when falling. Keep your arms and legs slightly bent as you fall.

Most importantly, protect your head. If falling forward, turn your face to the side. If falling backward, be sure to tuck your chin to your chest so your head does not hit the ground. Like the bull-riding cowboys who train to land on their hands and feet after being bucked off the bull, CKD patients or the elderly should learn how to step into balance when off balance to prevent falling. While these maneuvers may not always prevent a fall, they may be helpful for many to decrease the chances of falling.
This exercise will help you practice regaining your balance to prevent a fall. First, stand with both feet together. Beginners may hold onto a handrail to first practice the motions.

- Lean slightly forward until you feel off-balance.
- Step forward with one foot in front of you until you have reestablished balance. Repeat this ten times. Perform the same exercise with the other foot. Next, try stepping backward ten times, first with the left and then the right foot.
- Next, when feeling off balance, step across with one foot until you have reestablished balance.
- Finally, stand with your feet together, then lean to the side until you feel off-balance. Step to the side with one foot until you regain balance. When you feel comfortable, you can practice “falling” and regaining balance without holding onto anything.
Although we cannot rewind our chronological clocks, we can impact the effects of aging by reducing inflammation, eating healthier, and exercising[10]. For further information on falls, visit the CDC’s STEADI website, https://www. cdc.gov/steadi/. Falls in CKD patients are also discussed in “Staying Healthy with Kidney Disease.”[8]
Conclusion
Falls are a leading cause of death and common in the elderly and patients with chronic disorders, especially CKD. They can be mechanical or non-mechanical. Kidney patients should be assessed and if determined to be at risk for a non-mechanical fall, strategies should be developed to prevent falls.
Regardless of one’s fall risk, fall-proofing the home, wearing proper footwear, assuring vision is optimal, and getting into an exercise program to work on balance, muscle strength, and fall prevention, will not just improve one’s well-being but also help reduce the risk of injury in the event of a mechanical fall.
Tips to fall proof your home:
- Install and use grab bars in the bathroom and shower
- Be sure carpets and rugs are secure, slip-resistant, and padded
- Install nightlights
- Declutter pathways, especially before going to bed
- Use stairway handrails
- Get assistance if you need help, especially if you have gait disturbances, dementia, or balance disorders
Additional tips to prevent falls:
- Wear proper footgear
- Get your vision checked regularly
- Practice balance exercises and muscle strengthening exercises
References
1. Papakonstantinopoulou K, Sofianos I. Risk of falls in chronic kidney disease. J Frailty Sarcopenia Falls. 2017;2(2):33-8.
2. Fleming J, Matthews FE, Brayne C. Falls in advanced old age: recalled falls and prospective follow-up of over-90-year-olds in the Cambridge City over-75s Cohort study. BMC Geriatr. 2008;8:6. doi: 10.1186/1471-2318-8-6.
3. Livingston R, Koval L, Livingston L, Scholes N. Six-year retrospective study of bull-riding injuries in central Queensland. Australas Med J. 2012;5(7):362-6. doi: 10.4066/amj.2012.1280.
4. Todd C, Skelton D: What are the main risk factors for falls among older epople and what are the most effective interventions to prevent these falls? http://www.euro.who.int/document/E82552.pdf, (2004). Accessed 2004.
5. Mitch WE, Fadem SZ. Muscle Breakdown in Kidney Disease: Mechanisms and Management Strategies. In: Fadem SZ, editor. Staying Healthy with Kidney Disease: A Complete Guide for Patients. Cham: Springer International Publishing; 2022. p. 83-6.
6. Beaudart C, Zaaria M, Pasleau F, Reginster J-Y, Bruyère O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS One. 2017;12(1):e0169548. doi: 10.1371/journal.pone.0169548.
7. Nguyen ML, Fadem SZ. Exercises for People with Chronic Kidney Disease and Seniors. In: Fadem SZ, editor. Staying Healthy with Kidney Disease: A Complete Guide for Patients. Cham: Springer International Publishing; 2022. p. 87-101.
8. Fadem SZ. Falls in CKD Patients and Seniors: Causes and Prevention. In: Fadem SZ, editor. Staying Healthy with Kidney Disease: A Complete Guide for Patients. Cham: Springer International Publishing; 2022. p. 103-12.
9. Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750. doi: 10.1136/bjsports-2016-096547.
10. Fadem SZ. Aging: Challenges and Interventions. In: Fadem SZ, editor. Staying Healthy with Kidney Disease: A Complete Guide for Patients. Cham: Springer International Publishing; 2022. p. 15-7.
Photos by MishaFit
© 2022 Stephen Z. Fadem, MD All rights reserved.
Dr. Fadem is a champion for chronic kidney disease education. He is a Clinical Professor of Medicine, Baylor College of Medicine, Section of Nephrology. Dr. Fadem attended Tulane University and graduated from the University of Oklahoma College of Medicine. After he completed his internship and residency at the University of Texas Health Science Center – MD Anderson and Hermann Hospitals, he did a renal fellowship at the University of Texas Health Science Center, San Antonio. Dr. Fadem was one of the first doctors to discover the value of the internet for patient education, and founded several websites dedicated to public service and the dissemination of clinical information including The Nephron Information Center, Wikikidney, Touchcalc, and dialysisunits.com. He has participated heavily in the development and revisions of numerous AAKP patient education materials including the “AAKP Patient Plan” series and the “AAKP Kidney Beginnings: A Patient’s Guide to Living with Reduced Kidney Function.”
Dr. Fadem is the recipient of the National Kidney Foundation’s Distinguished Service Award, the AAKP Visionary Award, the AAKP Peter Lundin, MD Award, the AAKP Medal of Excellence, and the President’s Volunteer Service Award. Dr. Fadem is listed in America’s Top Doctors. He serves as editor of aakpRENALIFE magazine, and as historian for AAKP.
Misha (Michelle) L. Nguyen has been employed with Texas Children’s Hospital for 13 years and has her master’s degree in Healthcare Finance. Misha is also a personal trainer with certifications as a Senior Fitness Specialist and Weight Loss Specialist. Misha uses her positive energy to motivate and inspire her clients. In her spare time, she enjoys spending time with her family.

























